Acid-Base Disorders for NCLEX Exam
Important Concepts You Must Know to Pass:
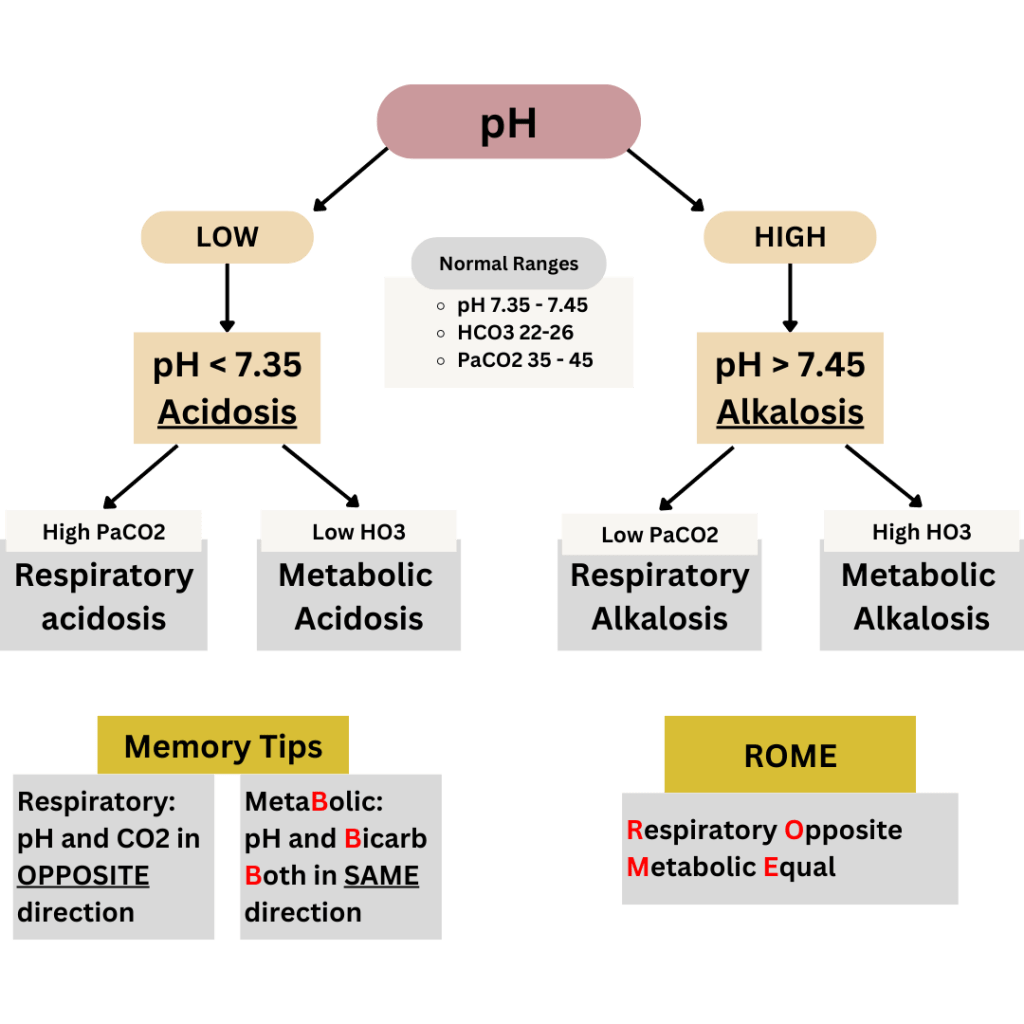
How to Identify the Type of Acid-Base Disorder
- Understand Normal Values for pH, CO2, and HCO3 (Bicarbonate)
It’s crucial to memorize these normal ranges to solve acid-base imbalance questions:- pH: 7.35 – 7.45
- CO2: 35 – 45 mmHg
- HCO3 (Bicarbonate): 22 – 26 mEq/L
- Determine if the Disorder is Acidotic or Alkalotic
Check the pH to see if the body is in an acidic or alkaline state:- pH < 7.35: Indicates acidosis (too much acid or too little base).
- pH > 7.45: Indicates alkalosis (too much base or too little acid).
- Identify if the Imbalance is Respiratory or Metabolic
Once you know if it’s acidotic or alkalotic, check the relationship between the pH and bicarbonate (HCO3) to determine the cause:- Use the “Rule of B’s”:
- If pH and Bicarb Both move in the same direction (either both increase or both decrease), it’s a Metabolic imbalance.
- If pH and Bicarb move in opposite directions, it indicates a Respiratory imbalance.
- Use the “Rule of B’s”:
NCLEX Tips: The NCLEX exam typically avoids overly complex or convoluted questions. Instead, it focuses on clear, straightforward scenarios that assess your fundamental nursing knowledge and decision-making skills.
Signs and Symptoms of Acid/Base Imbalances
Key Concept: “As the pH Goes, So Goes My Patient, Except for Potassium”
This phrase helps you remember how pH changes affect the body:
- When pH is low, everything slows down, except for potassium, which rises.
- When pH is high, everything speeds up, except for potassium, which drops.
Alkalosis (pH > 7.45)
- When the pH is high, most body systems become overactive:
- Symptoms:
- Tachycardia (fast heart rate)
- Tachypnea (rapid breathing)
- Hypertension (high blood pressure)
- Seizures, irritability, spasticity
- Diarrhea and increased bowel sounds (borborygmi)
- Hyperreflexia (exaggerated reflexes: 3+ or 4+)
- Potassium (K+): Hypokalemia (low potassium levels)
- Main Nursing Intervention: Prepare for suction to manage seizures.
- Symptoms:
Acidosis (pH < 7.35)
- When the pH is low, most body systems slow down:
- Symptoms:
- Bradycardia (slow heart rate)
- Bradypnea (slow breathing)
- Hypotension (low blood pressure)
- Constipation, absent bowel sounds
- Flaccidity, lethargy, coma
- Hyporeflexia (weak or absent reflexes: 0 or 1+)
- Potassium (K+): Hyperkalemia (high potassium levels)
- Main Nursing Intervention: Be ready to use an ambu bag or assist with intubation and ventilation to address respiratory arrest.
- Symptoms:
Quick Tip: “MAC Kussmaul”
- This helps you remember that Metabolic ACidosis is the only acid-base imbalance associated with Kussmaul respirations (deep, labored breathing).
Causes of Acid/Base Imbalance
Key Reminder: Don’t confuse the causes with the signs and symptoms!
1. If it Involves the Lungs, it’s Respiratory
- Ask yourself: Are they over-ventilating or under-ventilating?
- If UNDER-ventilating:
- The patient isn’t getting enough oxygen, causing CO2 buildup (which is acidic).
- This results in ACIDOSIS: choose pH < 7.35 (under-ventilating = lower pH).
- If OVER-ventilating:
- The patient is breathing too fast, losing too much CO2 (reducing acidity).
- This results in ALKALOSIS: choose pH > 7.45 (over-ventilating = higher pH).
2. If it’s Not Lung-Related, it’s Metabolic
- If the patient has prolonged vomiting or gastric suctioning (which removes stomach acid), this leads to metabolic alkalosis.
- For everything else (not related to the lungs or vomiting), assume it’s metabolic acidosis.
NCLEX Tips:
- If you’re unsure of the answer, consider “Metabolic Acidosis” as a possible default choice, as it’s commonly tested.
- Focus on the modifying phrases in the question rather than just the main noun or diagnosis, as these phrases often contain key details that guide your decision.
Ventilators
What is a Ventilator?
A ventilator is a machine that helps patients breathe when they are unable to do so adequately on their own. It moves air in and out of the lungs to support breathing. Ventilators have two important alarms: a high-pressure alarm and a low-pressure alarm.
High-Pressure Alarm
This alarm is triggered when there is increased resistance to airflow. This usually indicates an obstruction. Here’s what to check for:
- Kinks in the tubing → Straighten the tubing.
- Condensed water in the tube → Empty the water.
- Mucus plugs → Have the patient turn, cough, take deep breaths, and if necessary, suction them as needed (PRN).
Low-Pressure Alarm
This alarm is triggered when there is decreased resistance to airflow, which usually indicates a disconnection. Here’s what to check for:
- Main tube disconnection → Reconnect the tube unless it has fallen on the floor (in which case, replace it).
- Oxygen sensor disconnection → Reconnect the sensor unless it has fallen on the floor (replace if necessary).
Ventilator Settings
- If the ventilator is set too high (over-ventilating), the patient may develop Respiratory Alkalosis (characterized by rapid, shallow breathing or panting).
- If the ventilator is set too low (under-ventilating), the patient may develop Respiratory Acidosis (due to CO2 retention).