Calcium Channel Blockers (CCBs)
What are CCBs?
- CCBs are like “Valium” for your heart:
- Just as Valium calms your body, CCBs relax and slow down the heart.
- If the heart is experiencing tachycardia, tachyarrhythmia, or during a heart attack, the heart needs to rest, so you would give CCBs.
- However, if the patient is in shock or heart block, they need stimulation, so CCBs should NOT be given.
- Just as Valium calms your body, CCBs relax and slow down the heart.
- CCBs have negative effects on heart function:
- Negative inotropic: Weaken or reduce the force of heart contractions.
- Negative chronotropic: Slow down the rate of the heartbeat (decreased heart rate).
- Negative dromotropic: Slow the conduction of electrical impulses through the heart (from the SA node to the AV node).
- Positive ino/chrono/dromotropic effects = Cardiac stimulants (strong heartbeat).
- Negative ino/chrono/dromotropic effects = Cardiac depressants (weakened, slowed heart rate) = CCBs.
What do CCBs treat? Use “A, AA, AAA”:
- A: Antihypertensive – CCBs relax blood vessels, lowering blood pressure.
- AA: Antianginal – CCBs relax the heart and decrease oxygen demand, treating chest pain.
- AAA: Anti-Atrial Arrhythmia – CCBs treat atrial flutter, atrial fibrillation, premature atrial contractions (PACs), atrial bigeminy, and supraventricular tachycardia (SVT).
Side Effects of CCBs: Think “H-H”
- Headache – Due to vasodilation (commonly tested in SATA questions).
- Hypotension – As blood vessels relax, blood pressure can drop.
Examples of CCBs:
- Medications ending in -ZEM, -DIPINE, as well as verapamil, isoptin, and Cardizem (diltiazem).
- Cardizem can be administered via IV drip.
Nursing Considerations:
- Always assess and monitor BP before giving CCBs.
- If SBP is less than 100, hold the CCB.
- For Cardizem (diltiazem) given via IV drip, titrate the infusion rate depending on how low the SBP is.
Rhythm Strips You MUST Know
Key Terms:
- Tachycardia: Described as “bizarre.”
- Fibrillation: Described as “chaotic.”
- P wave: Indicates atrial activity.
- QRS depolarization: Indicates ventricular activity.
1. Normal Sinus Rhythm:
- P, QRS, and T waves present for every complex, with QRS complexes equally spaced.

2. Ventricular Fibrillation (VFIB):
- Chaotic QRS complexes with no pattern.

3. Ventricular Tachycardia (V Tach):
- Bizarre, wide QRS complexes with a pattern.

4. Asystole:
- A flat line, indicating a lack of QRS complexes.

5. Atrial Flutter:
- Rapid P wave depolarization, described as a “saw-tooth” pattern.
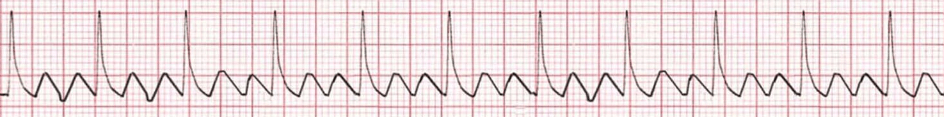
6. Atrial Fibrillation (AFIB):
- Chaotic P wave patterns.
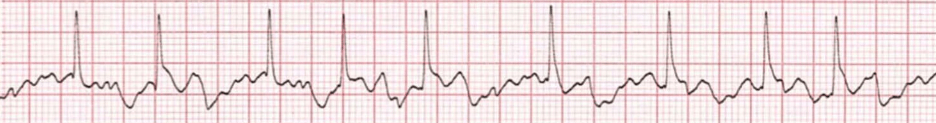
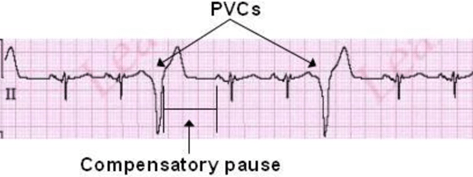
7. Premature Ventricular Contractions (PVCs):
- Periodic, wide, bizarre QRS complexes, typically of low priority.
- PVCs are common after an MI and are usually low priority, unless:
- 6 or more PVCs in a minute.
- 6 consecutive PVCs.
- R on T phenomenon (PVC falls on a T wave).
- These scenarios elevate PVCs to moderate priority, but never high priority.
Lethal Rhythms (High Priority)
- Ventricular Fibrillation (V-FIB) and Asystole are the most lethal rhythms.
- These rhythms result in low to no cardiac output, leading to no brain perfusion and can cause confusion or death within 8 minutes.
Cardiac Output (CO)
- No cardiac output = No pulse.
- Presence of cardiac output = Pulse is present.
Key Reminders:
- If a question refers to QRS Depolarization, it is referring to ventricular activity.
- If a question refers to P wave depolarization, it is referring to atrial activity.
Treatments for dysrhythmias
| Ventricular | Atrial | Lethal | ||
| PVCs (ventricular) | V-tach (ventricular) | Supraventricular Arrhythmia (atrial) | Ventricular Fibrillation (V-fib) or Pulseless Ventricular Tachycardia (V-tach) | Asystole |
| – Lidocaine – Amiodarone | Use the mnemonic “ABCD”: – Adenosine – Beta-blockers (medications ending in -lol) – Calcium Channel Blockers (CCBs) – Digoxin (Lanoxin) | Defibrillation (Shock) | – Epinephrine (first) – Atropine (second) | |
Atrial Treatments: “ABCD”
- Adenosine (Adenocard):
- Must be IV pushed in less than 8 seconds, followed by a 20 cc flush of normal saline.
- This can cause the patient to go into asystole for up to 30 seconds—don’t worry, the heart will restart.
- Beta-blockers (ending in -lol):
- Act like Valium for the heart, treating A, AA, AAA (Antihypertensive, Antianginal, Anti-Atrial Arrhythmia).
- They have negative inotropic, chronotropic, and dromotropic effects, similar to calcium channel blockers (CCBs).
- Side effects are headache and hypotension (“H-H”).
- Calcium Channel Blockers (CCBs):
- Also act like Valium for the heart and treat A, AA, AAA.
- CCBs are preferred over beta-blockers for patients with asthma/COPD, as they do not cause bronchoconstriction (beta-blockers do).
- Digitalis/Digoxin (Lanoxin):
- Be familiar with all these names and their cardiac effects.
Important Note:
- For IV push drugs, go slow unless you are administering adenosine, which requires a rapid push.
Chest Tube
Purpose of a Chest Tube:
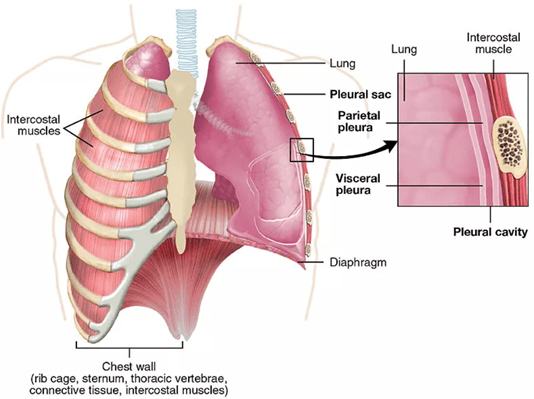
- The primary purpose of a chest tube is to re-establish negative pressure in the pleural space. Negative pressure helps the lungs adhere to the chest wall, allowing the lungs to expand when the chest wall moves.
- In the pleural space, negative pressure is beneficial (it keeps the lungs and chest wall together), while positive pressure pushes things apart.
Chest Wall vs. Lungs:
- The anatomical layers are as follows:
- Alveoli < Lung < Visceral pleura < Pleural cavity (space) < Parietal pleura < Chest wall.
- Normally, negative pressure in the pleural space keeps the lungs and chest wall together, ensuring the lungs expand with the chest’s rise and fall.
- In abnormal situations (e.g., air or blood in the pleural space), positive pressure disrupts this relationship and pushes the lungs away from the chest wall. A chest tube is inserted to remove the air or blood and restore negative pressure.
Conditions Treated with a Chest Tube:
- Pneumothorax: The chest tube removes air.
- In a pneumothorax, positive pressure is caused by the presence of air, so the chest tube removes the air to restore negative pressure.
- Hemothorax: The chest tube removes blood.
- In a hemothorax, positive pressure is caused by blood accumulating in the pleural space.
- Pneumohemothorax: The chest tube removes both air and blood.
- Pleural Effusion: A condition where fluid accumulates in the pleural space.
Closed Chest Drainage Devices
- Types: Common closed drainage devices include Jackson-Pratt, Pneumovac, Hemovac, etc.
- What to do if a drainage device is knocked over:
- Instruct the patient to take a deep breath and then set the device back upright.
- It is not a medical emergency; there’s no need to call the physician.
If the Water Seal of the Chest Tube Breaks:
- Clamp the chest tube (for less than 15 seconds) to prevent air from entering the chest.
- Cut the tube away from the broken system.
- Submerge the end of the tube in sterile water to create a temporary water seal.
- Unclamp the chest tube to allow air and fluid to escape. Clamping prevents air from entering but can also stop drainage, so it should only be done for less than 15 seconds.
- Important Note: The entire process—clamping, cutting, submerging, and unclamping—should be completed within 15 seconds.
If a Chest Tube Gets Pulled Out:
- Immediately cover the opening with a gloved hand (this is the first step).
- Then, apply a sterile Vaseline gauze and tape it on three sides (this is the best action to take).
Bubbling in the Chest Tube:
- Bubbling can be good or bad, depending on where and when it occurs.
- “In the water seal, continuous bubbling is bad.”
Analogies:
- Intermittent (like an in-and-out catheter): Similar to thoracentesis.
- Continuous (like a Foley catheter): Similar to a chest tube.
- Both Foley catheters and chest tubes have a higher risk of infection due to continuous drainage.
Rules for Clamping Chest Tubes:
- Do not clamp a chest tube for more than 15 seconds without a physician’s order.
- Use rubber-tipped clamps that won’t puncture the tubing, and always use double clamps.
- If the water seal breaks, the nurse has no more than 15 seconds to clamp, cut, submerge, and unclamp the tube.
Congenital Heart Defects (CHDs)
- Congenital heart defects are either “trouble” or “no trouble”—there’s no middle ground.
- Use the mnemonic “TRouBLe” (capital letters for consonants, lowercase for vowels) to remember that serious CHDs cause Trouble, are Right-to-left shunts, and are Blue (cyanotic).
| Pediatric Patients with “TRouBLe” Congenital Heart Defects (CHDs) | Pediatric Patients with “No Trouble” Congenital Heart Defects (CHDs) |
| These patients will require surgery soon or immediately to survive. They often experience slowed or delayed growth and development (failure to thrive). Shortened life expectancy is common. Parents will face significant emotional and financial stress and may go through periods of grief. The patient is likely to be discharged home with a cardiac monitor. After birth, the patient will typically stay in the hospital for a few weeks. The pediatrician or nurse will likely refer the patient to a pediatric cardiologist for specialized care. | These congenital heart defects are considered non-life-threatening and typically cause no major complications. |
| CHDs that cause “TRouBLe” often start with a T: – Tetralogy of Fallot – Truncus Arteriosus – Transposition of the Great Vessels – Tricuspid Atresia – Total Anomalous Pulmonary – Venous Return (TAPVR) – Exception: Left Ventricular Hypoplastic Syndrome – These defects involve a Right-to-Left blood shunt, causing cyanosis (blue discoloration). | These congenital heart defects are generally non-life-threatening and cause fewer complications: – Ventricular Septal Defect (VSD) – Patent Ductus Arteriosus (PDA) – Patent Foramen Ovale – Atrial Septal Defect (ASD) – Pulmonic Stenosis |
| Murmur: Both “TRouBLe” and “No Trouble” CHDs may present with a heart murmur. An echocardiogram is necessary to determine the cause of the murmur and assess the specific heart defect. | |
Tetralogy of Fallot (4 Defects): Use the mnemonic “PROVe” or “VarieD PictureS Of A RancH” to remember the four defects:
- Ventricular Septal Defect (VSD)
- Pulmonary Artery Stenosis
- Overriding Aorta
- Right Ventricular Hypertrophy
(No need to understand the specifics of these defects, just be able to recognize them as correct answer choices on the exam.)
Infectious Disease and Transmission-Based Precautions
There are four types of transmission-based precautions:
- Standard / Universal Precautions: Used for all patients to prevent the spread of infection through body fluids.
- Contact Precautions: For infections spread through direct or indirect contact (e.g., MRSA, C. diff).
- Droplet Precautions: For infections spread through large respiratory droplets (e.g., influenza, pertussis).
- Airborne Precautions: For infections spread through small airborne particles (e.g., tuberculosis, measles, varicella).
| Precautions | Infectious Diseases | PPE |
| Contact precaution | Enteric (GI/fecal-oral) infections: Include diseases like C. diff, hepatitis A, E. coli, cholera, and dysentery. Staph infections: Spread through direct contact. RSV (Respiratory Syncytial Virus): Spread via droplets that fall onto surfaces, which are then touched by the patient and potentially ingested. Do not cohort two RSV patients unless cultures and symptoms confirm they have the same strain. Herpes: Spread through direct contact with infected lesions or secretions. | Private room is recommended. Patients can be cohorted in the same room if matched by culture, not by symptoms. Order of donning PPE: Hand wash → gown → gloves. Use disposable supplies (e.g., gloves, paper plates, plastic utensils). Use dedicated equipment (e.g., stethoscope, BP cuff) and ensure it stays in the room, including toys if applicable. |
| Droplet precaution | – For infections spread via large respiratory droplets (from coughing or sneezing) that typically travel less than 3 feet. Examples include: – Meningitis – Haemophilus influenzae type B (e.g., epiglottitis—avoid inserting anything into the throat due to airway obstruction risk). | Private room is recommended. Patients can be cohorted in the same room if matched by both culture and symptoms. Order of donning PPE: Hand wash → mask → goggles or face shield → gloves. Use disposable supplies. Use dedicated equipment that stays in the room. |
| Airborne precaution | Use the mnemonic “MTV” for airborne precautions: M: Measles (MMR) T: Tuberculosis (TB) V: Varicella (chickenpox) | Private room is required. Patients can be cohorted in the same room if matched by both culture and symptoms. Order of donning PPE: Hand wash → goggles or face shield → gloves. Wear a mask when leaving the room. Keep the door closed at all times. Disposable supplies and dedicated equipment are recommended but not essential. Ensure the room has negative pressure airflow to prevent the spread of airborne particles. |
PPE
- Order for donning (putting on): Follow reverse alphabetical order, with the mask in the second position:
- Gown
- Mask
- Goggles
- Gloves
- Order for doffing (taking off): Follow alphabetical order:
- Gloves
- Goggles
- Gown
- Mask
Math Problems
- Dosage calculation: Follow standard formulas for medication doses.
- IV Drip Rates: Use the formula:
- IV drip rate = (volume × drop factor) / time
- Micro/mini drip sets: 60 drops/mL
- Macro drip sets: 10 drops/mL
- Pediatric dose: Remember the conversion—2.2 lbs = 1 kg.