Endocrine System – Focus on Thyroid & Adrenal Glands
Thyroid Gland
- Function: Regulates metabolism.
Hyperthyroidism
- Definition: “Hypermetabolism,” where the metabolism is elevated.
- Signs and Symptoms:
- Weight loss
- High heart rate (tachycardia) and blood pressure (hypertension)
- Irritability
- Heat intolerance, cold tolerance
- Exophthalmos: Bulging eyes
- Also Known As: Graves’ disease (“running yourself into the grave”).
Treatments for Hyperthyroidism
- Radioactive Iodine:
- Patient should be isolated for 24 hours (limit visitors).
- Handle urine carefully (flush 3 times); if spilled, call the hazmat team (urine is the primary radioactive risk).
- PTU (Propylthiouracil):
- Lowers thyroid activity (“Puts Thyroid Under”).
- Immunosuppressant: Monitor WBC count closely.
- Thyroidectomy (surgical removal):
- Total Thyroidectomy:
- Requires lifelong hormone replacement.
- Risk of hypocalcemia (due to possible removal of parathyroid glands) → watch for Trousseau’s sign and Chvostek’s sign.
- Subtotal Thyroidectomy:
- Does not require lifelong hormone replacement.
- Risk of Thyroid Storm post-op.
- Total Thyroidectomy:
Thyroid Storm (Crisis)
- Definition: A life-threatening condition that occurs with untreated or undertreated hyperthyroidism.
- Signs and Symptoms:
- Very high fever (≥105°F).
- Extremely high blood pressure (e.g., 210/180).
- Severe tachycardia (heart rate of 180-200).
- Psychotic delirium (medical emergency, can lead to brain damage).
- Treatment:
- Focus on cooling and oxygenation.
- First: Apply ice packs.
- Best: Use a cooling blanket.
- Oxygen at 10L via mask.
- Avoid Tylenol, as it won’t be effective.
- In sequence: oxygen → ice packs → cooling blanket.
- Never leave the patient unattended.
Post-Operative Risks for Thyroidectomy
- First 12 hours:
- Focus on airway and hemorrhage.
- 12-48 hours:
- Total Thyroidectomy: Watch for tetany (due to low calcium) as this can obstruct the airway.
- Subtotal Thyroidectomy: Watch for thyroid storm.
- After 48 hours (up to 72 hours):
- Risk of infection (but never prioritize infection as a risk in the first 72 hours post-op).
Hypothyroidism
- Definition: “Hypometabolism,” where the metabolism is decreased.
- Signs and Symptoms:
- Weight gain
- Cold intolerance, heat tolerance
- Low heart rate and blood pressure
- Myxedema: Severe hypothyroidism.
Treatment for Hypothyroidism
- Medication: Administer thyroid hormone replacement (Synthroid/Levothyroxine).
- Caution:
- Avoid sedating these patients; it can lead to coma.
- Pre-op consideration: Always question an order for sedatives like Ambien at bedtime.
- Ensure patients continue taking their thyroid medication, even if NPO (do not hold thyroid meds unless explicitly ordered).
ADRENOCORTEX Diseases (Start with A & C)
- Examples include Cushing’s, Conn’s, and Addison’s diseases.
Addison’s Disease
- Definition: Undersecretion of the adrenal cortex.
- Signs and Symptoms:
- Hyperpigmentation (tanned appearance).
- Inability to adapt to stress: These patients cannot increase blood glucose or blood pressure during stress, leading to dangerously low levels.
- Risk: Even minor stress (e.g., a dentist visit or fender bender) can lead to shock and death due to low blood pressure and glucose.
- Rare Condition: For every 600 Cushing’s patients, there is 1 Addison’s patient. (Example: JFK had Addison’s disease, and the stress of his injury contributed to his death.)
- Treatment: Glucocorticoids (steroids) such as prednisone, dexamethasone, and hydrocortisone.
- Memory Tip: In Addison’s disease, you need to “ADD a SONE” (steroids ending in “-sone”).
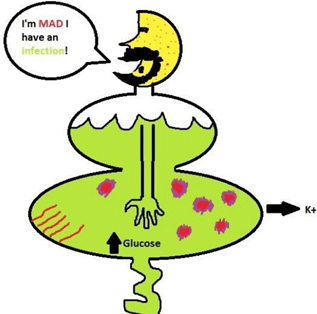
Cushing’s Disease
- Definition: Oversecretion of the adrenal cortex (“Cushy = More!”).
- Signs and Symptoms:
- Physical Appearance:
- Moon face (puffy, round face).
- Hirsutism (excessive facial hair).
- Truncal obesity (large abdomen with thin arms and legs due to muscle wasting).
- Buffalo hump (fat deposit on the upper back).
- Gynecomastia (breast development in men).
- Striae (stretch marks) and easy bruising.
- Fluid and Electrolyte Imbalance:
- Retains sodium and water, losing potassium.
- Emotional Symptoms: Irritability and mood swings.
- Immunosuppression: Prone to infections.
- Hyperglycemia: High blood glucose levels.
- Memory Tip: Think of “Cushman”—the classic presentation of Cushing’s.
- Physical Appearance:
- Treatment: Adrenalectomy (removal of the adrenal glands).
- Note: Bilateral adrenalectomy can lead to Addison’s disease, requiring lifelong steroids, potentially leading to a “Cushman” appearance again due to steroid use.
Laminectomy (Neuro)
- Definition: A surgical procedure that removes the lamina (the back part of the vertebra) to relieve pressure on the spinal cord or nerves. This is also known as decompression surgery.
Why is a Laminectomy Done?
- Purpose: To relieve nerve root compression.
- Signs of Nerve Root Compression (The 3 P’s):
- Pain
- Paresthesia (numbness and tingling)
- Paresis (muscle weakness)
Key Consideration: Location
- The location of the laminectomy is crucial in neuro questions.
- Common Locations:
- Cervical (neck)
- Thoracic (upper back)
- Lumbar (lower back)
Pre-Op Assessment Based on Location:
- Cervical (neck): Assess airway and function of arms/hands.
- Thoracic (upper back): Assess cough reflex and bowel function.
- Lumbar (lower back): Assess bladder function (e.g., when they last voided) and leg function.
Post-Op Care (Spinal Surgery)
- Log roll the patient (maintain spinal alignment).
- Don’t dangle the patient’s legs.
- Avoid sitting for longer than 30 minutes.
- Patients can walk, stand, and lie down without restriction.
Potential Complications Based on Location:
- Cervical: Risk for pneumonia.
- Thoracic: Risk for pneumonia and paralytic ileus.
- Lumbar: Risk for urinary retention and leg issues.
Discharge Teaching
Temporary Restrictions (for 6 weeks):
- Do not sit for more than 30 minutes.
- Lie flat and log roll when moving.
- No driving.
- No lifting more than 5 pounds (equivalent to a gallon of milk).
Permanent Restrictions:
- Never lift objects by bending at the waist.
- Cervical laminectomy patients: Do not lift anything over the head.
- Avoid activities involving jerking (e.g., horseback riding, roller coasters).
Additional Terminology:
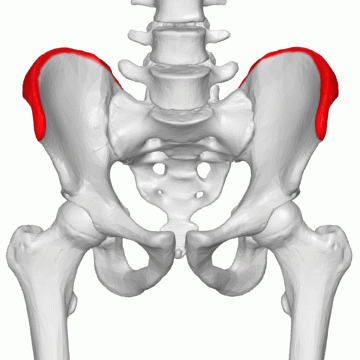
- Anterior Thoracic Laminectomy: Access through the chest to the spine.
- Laminectomy with Fusion: Involves a bone graft from the iliac crest (hip) with two incisions—one on the hip and one on the spine.
- Hip incision: More pain, bleeding, and drainage.
- Both incisions: Equal risk of infection.
- Spinal incision: Highest risk of graft rejection.
Key Reminder:
- The most important thing in any neuro question is the location of the laminectomy.