Rules for Prioritization
- Acute conditions take priority over chronic conditions.
- Fresh post-op (<12 hours) takes priority over acute or chronic medical/surgical patients.
- Unstable patients take priority over stable patients.
- Unstable patients include those with:
- Acute illness.
- Post-op less than 12 hours.
- General anesthesia within the first 12 hours.
- Lab abnormalities in C or D levels (e.g., INR in the 4s, K in the 6s, pH in the 6s, CO₂ in the 50s, low O₂ sat, high WBC, low ANC, low CD4, low platelets).
- Newly diagnosed, newly admitted, admitted <24 hours, or patients with changing or changed assessments.
- Experiencing unexpected signs and symptoms.
- Stable patients include those with:
- Chronic illness.
- Post-op more than 12 hours.
- Local or regional anesthesia.
- Lab abnormalities in A or B levels (e.g., elevated creatinine, BUN, Hg 8-11, bicarb, elevated Hct, elevated BNP, elevated Na, or low RBCs).
- Ready for discharge or being discharged.
- Unchanged assessments.
- Experiencing typical, expected signs and symptoms of their diagnosed disease.
- Unstable patients include those with:
Four Factors That Always Make a Patient Unstable, Even if Expected:
- Hemorrhage (but not simple bleeding).
- High fever (over 40°C) – This can lead to seizures.
- Hypoglycemia – This can cause brain damage.
- Pulseless or breathless – Conditions like ventricular fibrillation (V-fib) or asystole.
- Exception: At the scene of an unwitnessed accident, pulseless and breathless patients are considered low priority because they are likely deceased.
Mass Casualty Incident – Black Tag Criteria
In a mass casualty event, the following conditions result in a black tag (indicating the patient will not receive immediate care):
- Pulseless.
- Breathless.
- Fixed and dilated pupils (even if the patient is still breathing, they are considered a black tag and treated last).
Tie-Breaker Rule
If the rules for prioritizing based on acute vs. chronic, post-op time, or stable vs. unstable result in a tie, use the following guide:
- The more vital the organ, the higher the priority.
- Order of organ importance:
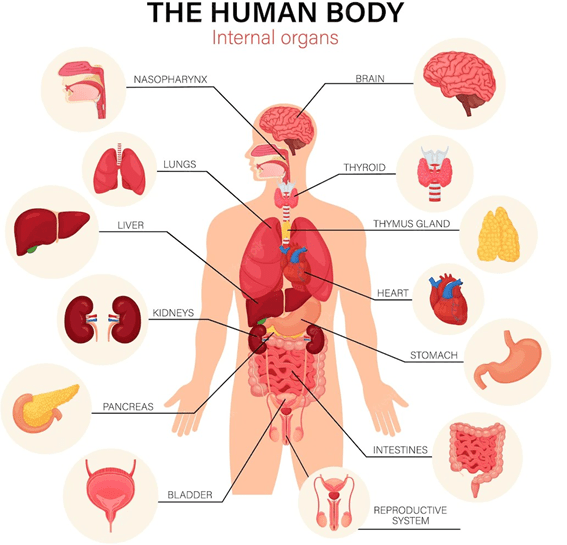
Brain > lung > heart > liver > kidney > pancreas.
- Order of organ importance:
- Important: Use this rule based on the organ involved in the modifying phrase, not the diagnosis.
Examples:
- A) 23-year-old male with CHF and K+ 6.6, no EKG changes.
- Chronic (low priority) / K+ 6.6 (high priority) / No changes (low priority).
- B) Patient with CKD and creatinine 24.7, pink frothy sputum.
- Chronic (low priority) / Creatinine elevated but expected (low priority) / Pink, frothy sputum (unexpected, high priority—lungs).
- C) Patient with acute hepatitis, jaundice, increased ammonia, you cannot arouse.
- Acute (high priority) / Expected symptoms (jaundice) (low priority) / Inability to arouse (unexpected, high priority—brain involvement).
Conclusion:
- C is the highest priority because of the brain involvement (the most vital organ), making it more urgent than A and B.
Delegation of Responsibility
| RN | LPN | UAP |
| First of anything: The RN handles the initial assessment, intervention, or task. Judgment: Any task requiring clinical judgment falls under the RN’s responsibility. Education: The RN is responsible for patient education. Assessment: The RN conducts all assessments, especially initial and complex assessments. Analysis: The RN analyzes patient data and outcomes. Critical Thinking: The RN is responsible for critical thinking and decision-making. Nursing Process: The RN handles the full nursing process: –Assessment, Diagnosis, Planning, Intervention, Evaluation. Accountability: The RN is accountable for any care provided by unlicensed assistive personnel (UAP) and must supervise and ensure tasks are done correctly. | IV Responsibilities: LPNs can maintain an IV and document flow, but cannot initiate or adjust IV therapy. Care Plans: LPNs can implement a care plan but cannot create one. Tasks: LPNs handle monitoring, reinforcing teaching, routine workups, and specific assessments (such as ostomy care). Patient Population: LPNs are responsible for stable patients only. Routine Procedures: LPNs can perform routine procedures, including: – Catheterization. – Administering medications (excluding IV meds). – Ostomy care and enteral feeding. – Maintaining tube patency. – Nasotracheal suctioning and nasogastric tube insertion. – Dressing changes. – Administering subcutaneous (subQ), intramuscular (IM), and oral medications. Nursing Process: LPNs do not engage in the full nursing process (e.g., they do not assess, diagnose, or evaluate). | Activities of Daily Living (ADLs): UAPs can assist with tasks like bathing, dressing, and feeding. Hygiene: UAPs help with personal hygiene tasks such as oral care, bathing, and toileting. Linen Changes: UAPs are responsible for changing bed linens and keeping the patient’s environment clean. Routine and Stable Vital Signs: UAPs can take and document vital signs for stable patients. Collecting and Documenting Intake & Output (I&O): UAPs can track and document a patient’s fluid intake and output. Blood Glucose Checks: UAPs can perform sugar checks for diabetic patients. Positioning and Range of Motion (ROM): UAPs can assist with positioning and perform passive and active range of motion (ROM) exercises. Nursing Process: UAPs are not involved in the nursing process (they do not assess, diagnose, or evaluate). |
New Graduate Nurse Responsibilities
Stable Patients:
- New graduates are typically assigned stable patients.
LPN Restrictions:
LPNs cannot do the following:
- Start an IV.
- Hang or mix IV medications.
- Push IV medications.
- Administer blood or handle central lines (e.g., flushing or changing dressings).
- Create care plans (but they can implement pre-existing care plans).
- Provide or develop teaching (they can only reinforce teaching that has already been provided).
- Care for unstable patients.
- Perform the first of anything, including:
- Creating a care plan.
- Conducting the initial assessment.
- Changing the first dressing, ambulating for the first time, or obtaining the first post-op vital signs.
- Performing the first assessment after a change in the patient’s condition.
- Assessments: LPNs cannot perform initial assessments for admission, discharge, transfer, or after a significant change in condition.
UAP Restrictions:
UAPs cannot do the following:
- Charting: UAPs can only chart what they did, not what they observed or assessed about the patient.
- Example: They can document, “side rail is up, bed is lowered,” but they cannot chart, “patient less anxious, tolerated ambulation well.”
- Medication administration: UAPs can only give topical, over-the-counter (OTC) medications like barrier creams (e.g., ADG creams).
- UAPs cannot administer medications like nitroglycerin or prescription ointments (e.g., Neosporin, hydrocortisone).
- Assessments: UAPs can only take vital signs or perform blood sugar checks (accu-checks).
- Treatments: UAPs can assist with basic treatments, such as administering enemas.
What to Delegate and Not Delegate to Family Members/Friends of Patients
- Never delegate safety responsibilities to family members or friends of the patient.
- If a family member asks to help while you, the RN, are away, you cannot delegate any task related to patient safety.
- You cannot delegate safety tasks to non-hospital caregivers unless they have been trained for that specific task.
- If training is provided, the RN must document what was taught in the patient’s record.
- Example:
- Can a mother give insulin shots to her 3-year-old child?
- Yes, but only if you have properly trained her and documented the teaching in the chart.
- If a new mother asks the RN to leave the baby’s crib rail down while she bathes the baby and says she’ll put it up later:
- The RN should respond by staying with the mother until the rail is safely up.
- Do not delegate this safety responsibility to the family.
- Can a mother give insulin shots to her 3-year-old child?
Staff Management: How to Handle Inappropriate Behavior from Staff
This section deals with managing inappropriate behavior, not prioritizing or delegating tasks.
- Four response options when dealing with staff behavior:
- Tell the supervisor.
- Confront the staff member and take over the task immediately.
- Talk to the staff member later.
- Ignore it (Never ignore inappropriate behavior—this is the wrong answer as it’s important to use these moments as teaching opportunities).
How to Choose the Correct Response:
- Is the staff member doing something illegal?
- If yes, tell the supervisor immediately.
- If no, ask yourself the next question.
- Is anyone in immediate physical or psychological harm?
- If yes, confront the staff member immediately and take over the task.
- If no, ask yourself the next question.
- Is this behavior simply inappropriate (but not harmful)?
- If yes, talk to the staff member later about the incident.
Special Scenario:
- If the behavior is both illegal and harmful to the patient, confront the staff member immediately, take over the task, and then report it to the supervisor.
Organ location (know the organ locations)
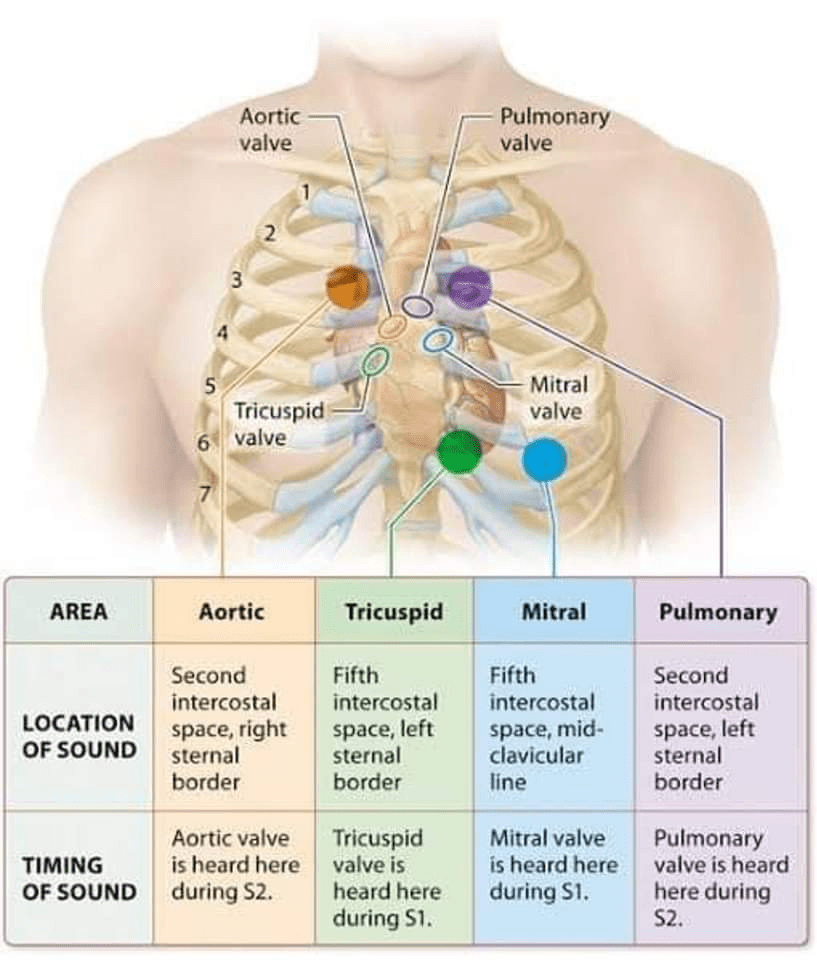
Auscultating Over Heart Valves
When identifying heart valve locations, you must place the stethoscope precisely over the correct area. The areas for auscultation of murmurs or heart sounds can be remembered with the mnemonic “A PET M”:
- Aortic Valve:
- Located in the 2nd intercostal space, to the right of the sternal border.
- Pulmonic Valve:
- Located in the 2nd intercostal space, to the left of the sternal border.
- Erb’s Point (rarely tested on NCLEX):
- Located in the 3rd intercostal space, to the left of the sternal border, between the pulmonic and tricuspid valves.
- Tricuspid Valve:
- Located in the 4th intercostal space, to the left of the sternal border.
- Mitral Valve:
- Located in the 5th intercostal space, at the midclavicular line.
- The apical pulse is located at the same spot as the mitral valve auscultation point.
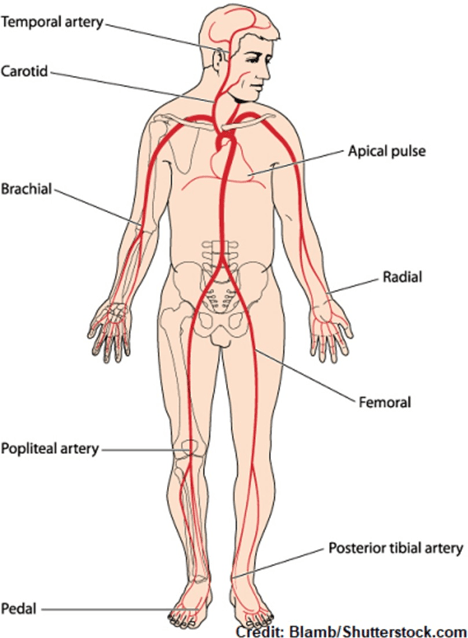
Palpating for pulses (know where on the body these pulses are located)
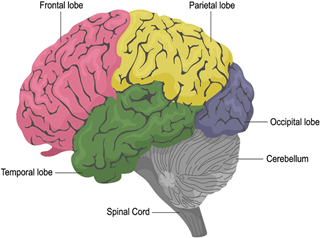
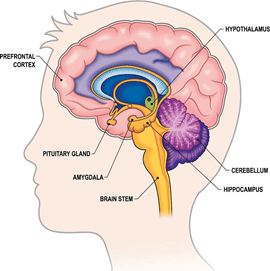
Brain Anatomy
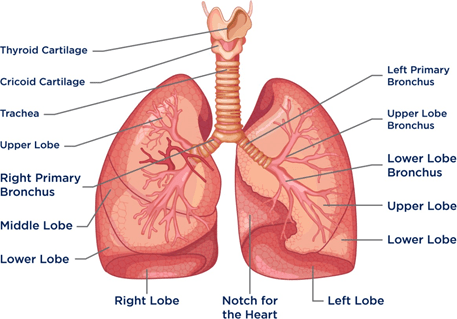
Lungs Anatomy
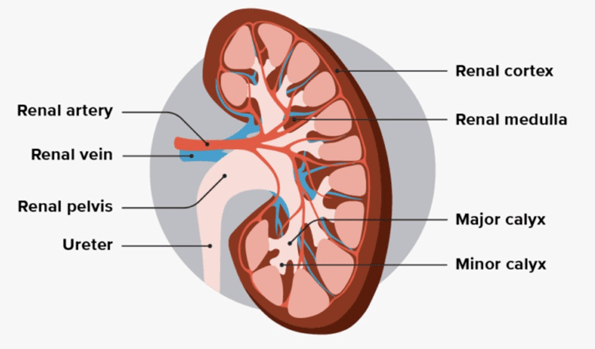
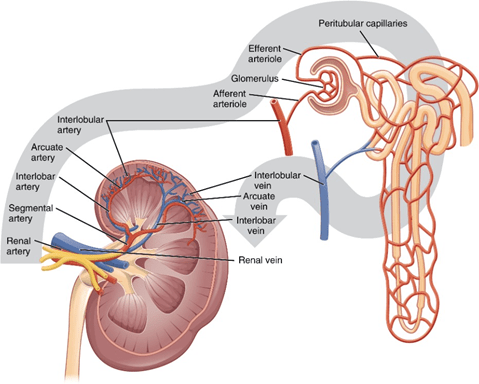
Kidneys Anatomy