Key Concepts to Remember
Cullen’s Sign:
- Description: Bruising around the umbilical area, indicating intraperitoneal bleeding.
Grey-Turner’s Sign:
- Description: Bruising on the flank, a sign of retroperitoneal bleeding.
Kehr’s Sign:
- Description: Sharp pain in the left shoulder due to diaphragm irritation, often associated with abdominal injury.
Abdominal Trauma
- Signs:
- Umbilical bruising: Suggests intraperitoneal hemorrhage.
- Flank bruising: Indicates retroperitoneal bleeding.
Abdominal Compartment Syndrome (ACS)
- Characteristics: Can occur without noticeable distention.
- Common Triggers: Trauma, emergency abdominal surgeries, massive fluid resuscitation.
- Effects of Increased Intra-Abdominal Pressure (IAP):
- Reduced cardiac output.
- Increased systemic vascular resistance (SVR).
- Decreased renal perfusion and venous return.
Monitoring: Bladder pressure measurement.
- Normal: 0–5 mmHg.
- Hypertension: >12 mmHg.
- Decompression laparotomy required: >20 mmHg.
- Fatal threshold: >25 mmHg.
Prevention for IAP > 12 mmHg:
- Elevate the head of bed < 20° or use reverse Trendelenburg.
- Manage pain and agitation.
- Loosen tight clothing.
- Avoid hypervolemia.
- Use NGT with low intermittent wall suction (LIWS).
- Check for bowel impaction.
Esophageal Varices
- Cause: Portal hypertension, often linked to liver disease.
- Treatment:
- Endoscopy with banding or sclerotherapy.
- Esophageal balloon (Sengstaken-Blakemore tube):
- Inserted nasally or orally.
- Inflated to compress blood flow and stop bleeding.
- Caution: Airway obstruction if displaced—scissors must be kept bedside to deflate the balloon immediately.
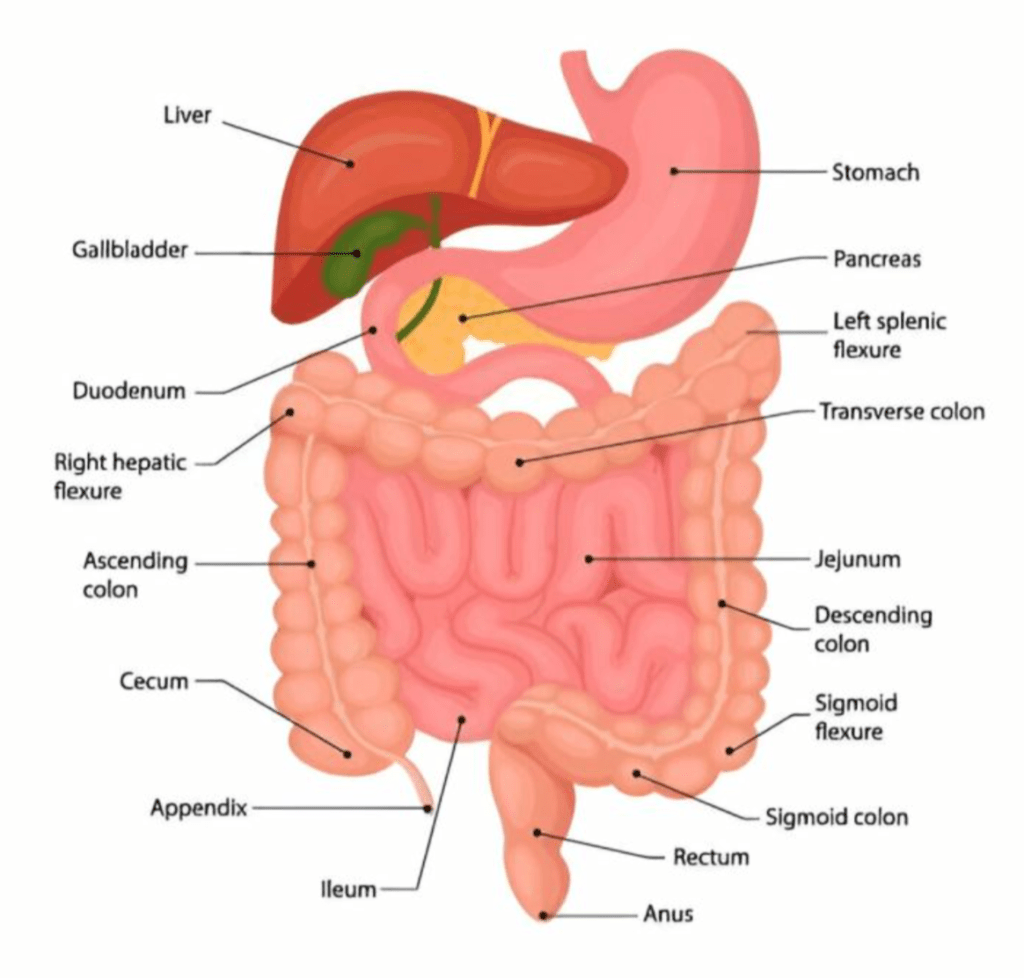
Bowel Infarction
- Cause: Decreased blood supply to mesenteric vessels, potentially leading to necrosis, perforation, or peritonitis.
- Treatment: Gastric decompression via NGT and bowel resection if needed.
Bowel Obstruction
- Small Bowel: Sharp, intermittent pain, early vomiting, high-pitched bowel sounds.
- Large Bowel: Dull pain, late vomiting, low-pitched sounds, abdominal distention.
- Progression: Hyperactive bowel sounds early, hypoactive or absent late.
- Treatment: NGT, fluid replacement for hypovolemia, and pain management.
Bowel Perforation
- Signs: Rigid abdomen, rebound tenderness, absent bowel sounds.
- Treatment: Antibiotics after cultures and urgent surgery.
Liver Failure
Chronic Liver Failure:
- Common Cause: Alcohol use disorder.
- Key Considerations: Avoid lactated Ringer’s solution to prevent lactic acidosis.
Ammonia Levels:
- Elevated ammonia (NH3) can lead to encephalopathy and increased ICP.
- Management:
- Lactulose to lower ammonia.
- Neomycin or rifaximin to reduce gut bacteria.
- Management:
Acute Liver Failure:
- Cause: Acetaminophen overdose.
- Treatment: N-acetylcysteine (Mucomyst).
Labs in Liver Failure:
- Increased: AST, ALT, bilirubin, NH3.
- Decreased: Albumin, protein, blood glucose.
Symptoms: Altered mental status, asterixis, ascites, jaundice, renal failure (hepatorenal syndrome).
Acute Pancreatitis
- Cause: Pancreatic inflammation and autodigestion.
- Symptoms:
- Boring pain radiating across quadrants.
- Nausea, vomiting, rigid abdomen, absent bowel sounds.
- Hemorrhagic signs: Cullen’s (umbilicus) and Grey-Turner’s (flank).
- Complications:
- Left lobe atelectasis, left pleural effusion, ARDS.
- Systemic inflammatory response syndrome (SIRS).
- Labs: Elevated amylase, lipase, glucose; decreased calcium.
Management:
- NGT, fluid/electrolyte therapy, pain control (morphine), PPIs, H2 blockers.
Spleen Injury
- Cause: Typically blunt abdominal trauma.
- Signs of Rupture: Kehr’s sign, abdominal distension, absent bowel sounds.
- Treatment: Supportive care and monitoring for sepsis.
Nutrition
Enteral Nutrition
- Benefits: Preferred over TPN, prevents malabsorption.
- Timing: Initiate within 24–48 hours.
- Key Points:
- Bowel sounds and resolved ileus are not prerequisites.
- Confirm tube placement via x-ray.
- Keep the head of the bed elevated >30°.
Total Parenteral Nutrition (TPN)
- Timing:
- Begin after 7 days if the patient was previously well-nourished.
- Start immediately if malnourished.