Shock
A state in which cells become dysfunctional due to insufficient oxygen supply or the inability to utilize oxygen effectively.
Three Primary Stages of Shock
A. Initial/Compensatory Stage (EARLY PHASE)
- The sympathetic nervous system (SNS) and renin-angiotensin-aldosterone system (RAAS) become activated to maintain perfusion.
- Reduced cardiac output (CO) or low oxygen levels trigger vasoconstriction.
- The body compensates to maintain blood pressure (BP).
- Signs & Symptoms: No significant change in BP, restlessness, rapid heart rate, increased respiratory rate.
B. Progressive Stage (ONSET OF HYPOTENSION)
- Compensatory mechanisms begin to fail, leading to a drop in BP.
- Signs & Symptoms: Worsening tachycardia, metabolic acidosis, declining PaO2, altered mental status (AMS), and skin becoming cold, clammy, or mottled.
C. Refractory Stage (ADVANCED/FINAL PHASE)
- The body no longer responds to treatment interventions.
- Even if shock is reversed, death may occur due to multiple organ dysfunction syndrome (MODS).
- Severe systemic hypoperfusion leads to:
- Neurological effects – encephalopathy, stroke
- Cardiac failure – ischemia, heart dysfunction
- Pulmonary complications – acute respiratory distress syndrome (ARDS)
- Liver failure
- Renal failure – acute tubular necrosis (ATN)
- Hematologic disorders – disseminated intravascular coagulation (DIC)
Types of Shock
Cardiogenic Shock
- Most severe form of heart failure (HF).
- The heart is unable to pump effectively, leading to low cardiac output.
- Narrow pulse pressure is a key indicator.
- Treatment Focus:
- Increase heart function while reducing its workload.
- Use positive inotropes to enhance contractility.
- Reduce preload and afterload with vasodilators, intra-aortic balloon pump (IABP), or ventricular assist devices (VAD).
- Supplemental oxygen or mechanical ventilation as needed.
Hypovolemic Shock
- Occurs due to a severe reduction in circulating blood volume.
- Can be classified as hemorrhagic (blood loss) or non-hemorrhagic (fluid loss).
- Causes:
- Internal: Fluid shift into tissues (third-spacing).
- External: Gastrointestinal losses, renal fluid loss, burns, or hemorrhage.
- Signs & Symptoms: Low blood pressure (↓BP), narrow pulse pressure (<40 mmHg).
- Treatment Focus:
- Identify and address the cause.
- Immediate volume replacement (blood products or isotonic fluids like 0.9% NS/LR).
- Avoid vasopressors initially as they increase systemic vascular resistance (SVR), worsening hypoperfusion.
- Maintain key perfusion targets:
- Mean arterial pressure (MAP) > 65 mmHg
- Central venous pressure (CVP) between 6-10 mmHg
- Urine output > 0.5 mL/kg/hr
Sepsis & Septic Shock
- Focus on preventing multiple organ failure (MODS).
- Leading cause of death in non-cardiac intensive care units (ICUs).
- Affects multiple body systems, requiring comprehensive management.
Systemic Inflammatory Response Syndrome (SIRS)
- Diagnosed when two or more of the following criteria are met:
- Body temperature <36°C or >38°C
- Heart rate exceeding 90 beats per minute
- Respiratory rate over 20 breaths per minute
- White blood cell count outside the normal range (<4,000 or >12,000)
Sepsis
- SIRS criteria met along with a suspected infection.
- No indication of organ dysfunction.
Severe Sepsis
- Sepsis accompanied by signs of organ impairment, including:
- Altered level of consciousness (LOC)
- Decreased blood pressure (BP)
- Low oxygen levels (hypoxemia)
- Lactate levels above 2 mmol/L
- Reduced urine output (UOP)
Septic Shock
- Severe sepsis that persists despite fluid resuscitation, characterized by:
- Mean arterial pressure (MAP) below 65 mmHg despite adequate fluid administration OR requiring vasopressors.
Treatment Goals:
- Achieve and maintain MAP > 65 mmHg
- Restore normal mental status and heart rate
- Control the infection
- Administer fluids (30mL/kg crystalloid solution) for resuscitation
- Use vasopressors if blood pressure remains low:
- First choice: Norepinephrine (LEVO)
- Second choice: Vasopressin (VASO)
- Start broad-spectrum antibiotics immediately after obtaining blood cultures
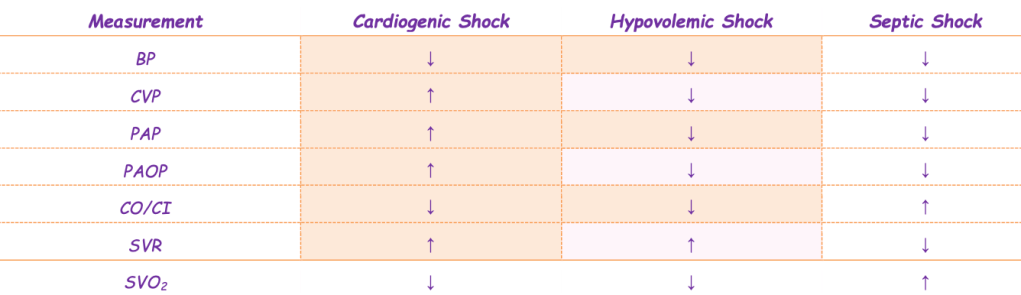
- Increased central venous oxygen saturation (SVO₂) in septic shock occurs because cells fail to properly utilize oxygen from the bloodstream.
- Elevated cardiac output (CO) and cardiac index (CI) in septic shock result from a compensatory increase in heart rate.
- Reduced systemic vascular resistance (SVR) in septic shock is caused by widespread blood vessel dilation.
- Higher systemic vascular resistance (SVR) in hypovolemic shock occurs due to blood vessel constriction compensating for fluid loss.
Trauma Response
- Can be a critical or fatal event, requiring rapid assessment and intervention.
- Evaluation follows a two-stage process:
Primary Assessment (ABCDE Approach)
- Airway – Ensure a clear airway using oral or nasal adjuncts if necessary.
- Breathing – Provide 100% oxygen and assist ventilation as needed.
- Circulation – Establish two large-bore IV lines and initiate fluid resuscitation.
- Disability – Assess level of consciousness (LOC), motor/sensory function (CMS), and Glasgow Coma Scale (GCS).
- Exposure – Ensure patient safety and monitor body temperature.
Secondary Assessment (FGHI Approach)
- Full set of vital signs – Continuously monitor the patient.
- Provide comfort measures – Address pain and distress.
- History collection – Identify medications, allergies, and relevant medical conditions.
- Thorough inspection – Examine the entire body, ensuring no injuries are overlooked.
Toxic Ingestion & Overdose Management
- If the patient is unresponsive, initiate treatment that addresses potential underlying causes.
- Naloxone (2mg) → Suspected opioid overdose
- Dextrose 50% → Possible hypoglycemia
- Thiamine (50-100mg) → Alcohol-related conditions
- Acetaminophen overdose → Administer N-acetylcysteine
- Alcohol toxicity → Use gastric lavage, IV fluids, and thiamine
- Benzodiazepine overdose → Administer flumazenil (Romazicon) and ensure airway protection
- Beta-blocker overdose → Treat with epinephrine and sodium bicarbonate
- Carbon monoxide poisoning → Provide 100% oxygen therapy
- Cocaine toxicity → Use benzodiazepines and vasodilators
- Cyclic antidepressant overdose → Treat with activated charcoal
- Ethylene glycol poisoning → Administer ethanol or initiate hemodialysis
- Opioid toxicity → Naloxone administration and airway support
- Aspirin overdose → Use activated charcoal or hemodialysis if necessary
Sedation & Pain Management
- Analgesics are administered before sedatives or anxiolytics.
- First-choice IV pain medications: Hydromorphone (Dilaudid), Morphine, and Fentanyl
- Monitor for side effects: Decreased respiratory rate and hypotension
- Sedation options: Lorazepam (Ativan), Midazolam (Versed), Propofol, and Dexmedetomidine (Precedex)
- Maintain a light level of sedation (RASS score 0 to -2)
- For continuous infusions, conduct a daily sedation break.
- If the patient does not tolerate sedation reduction:
- Increased agitation, rapid breathing, difficulty breathing, oxygen levels <90%, or hypotension
Targeted Temperature Management (TTM)
- Lowers brain metabolic activity and oxygen consumption.
- Inclusion criteria:
- Cardiac arrest witnessed, with downtime under 60 minutes
- Return of spontaneous circulation (ROSC)
- Unresponsive and not following commands (GCS <8)
Three Phases of TTM:
➢ Cooling Phase
- Start cooling immediately
- American Heart Association (AHA) recommends target temperature of 32-36°C
- Consider: Elevated glucose, low potassium, and shifts in electrolytes/fluids
➢ Maintenance Phase
- Maintain target cooling temperature for 24 hours
- Consider: Insulin infusion, sedation, or paralytics for shivering control
- Shivering increases oxygen consumption
- Monitor using Train-of-Four (TOF), aiming for 1-2 twitches
➢ Rewarming Phase
- Slowly increase body temperature at 0.5-1°C per hour
- Stop potassium infusions at least 8 hours before rewarming to prevent rebound hyperkalemia
- Discontinue sedation and paralytics
- Perform frequent neurological assessments