Eye Anatomy and Function

- Macula – Essential for sharp, central vision.
- Optic Disc – A slightly depressed, saucer-shaped area where the optic nerve exits; the cup-to-disc ratio should be less than 0.5, maintaining a balance between intraocular and intracranial pressure.
- Veins – Appear prominent and show pulsations under normal conditions.
- Papilledema – Swelling of the optic disc with indistinct margins, often caused by increased intracranial pressure (ICP), and loss of venous pulsations.

- Angle-Closure Glaucoma – Characterized by an excessively cupped optic disc due to elevated intraocular pressure; cup-to-disc ratio exceeds 0.5.
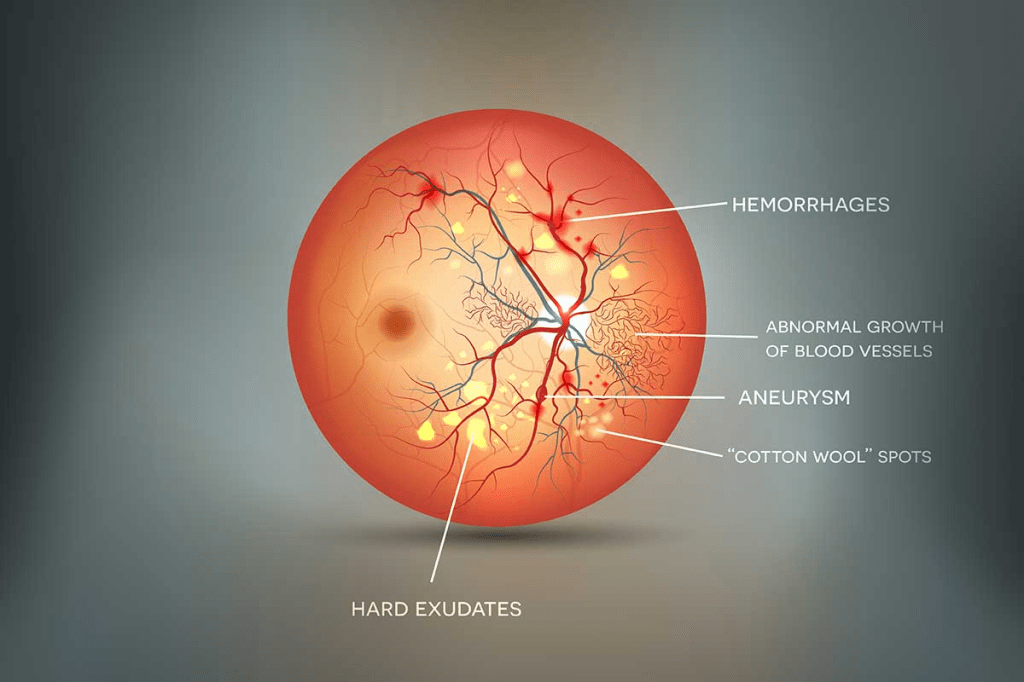
- Hypertensive Retinopathy
- Hardened arterioles appear as copper or silver wires.
- AV Nicking – When an artery compresses a crossing vein, often indicating retinal atherosclerosis.
- Flame-Shaped Hemorrhages – Indicative of retinal bleeding caused by hypertension.

Eye Examination
- Visual Acuity Testing – Essential for any eye-related symptoms.
- OU (both eyes), OD (right eye), OS (left eye).
- A two-line discrepancy between the eyes may indicate an issue.
- Up to two errors per line are acceptable.
- Legal blindness is defined as 20/200 vision.
- By age six, normal vision reaches 20/20.
- Slit-Lamp or Binocular Loupe – Assesses the anterior eye structures, including the cornea, conjunctiva, sclera, and iris.
- Use a penlight to examine at a 180-degree angle.
- Fluorescein Staining – Identifies corneal abrasions or ulcers.
- Lid Eversion – Necessary for inspecting the undersurface of the eyelids.
- Near Vision Test – Have the patient read fine print.
- Key Signs of an Ophthalmic Emergency:
- Redness, pain, and sudden vision changes.
- Presbyopia – A gradual age-related decline in the ability to focus on close objects, due to lens stiffening, typically beginning around age 40.
- Amsler Grid Test – Detects early macular degeneration.
- Tonometry – Measures intraocular pressure (IOP) to screen for glaucoma.
- Foreign Object Protrusion – Should never be removed in a non-clinical setting.
Diabetic Retinopathy
- Microaneurysms – Small bulging areas in retinal blood vessels.
- Cotton Wool Spots – Areas of retinal nerve fiber damage.
- Flame Hemorrhages – Bleeding in the retina, often linked to diabetic changes.
Cataracts
- Risk Factors: Chronic steroid use, trauma, aging, excessive sun exposure, and smoking.
- Lens Opacity: Can develop centrally or peripherally.
- Symptoms: Increased sensitivity to glare (especially from headlights at night or sunlight), halos around lights, and progressive blurring of vision.
- Clinical Findings:
- Absent red reflex – Key diagnostic sign.
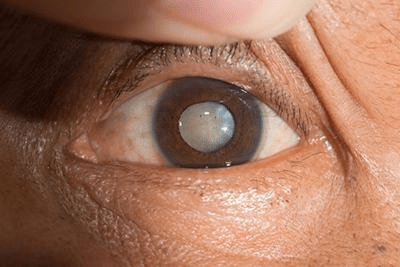
- Retinoblastoma Indicator: Leukocoria (white reflex) instead of the normal red reflex.
Eye Terminology
- Palpebral Conjunctiva – The mucous membrane lining the inner surface of the eyelids.
- Bulbar Conjunctiva – The mucous membrane covering the eyeball.
- Hyperopia (Farsightedness): Clear distance vision but difficulty focusing on close objects.
- Myopia (Nearsightedness): Clear near vision but blurry distance vision.
- Xanthelasma: Yellowish plaques near the inner corners of the eyelids; seen in about 50% of individuals with elevated lipid levels.
- Uveitis: Characterized by a dull, painful, red eye with visual disturbances.
- Key Features: Constricted, nonreactive, and irregularly shaped pupil.
- Management: Pupil dilation, corticosteroid treatment, and evaluation for an underlying autoimmune condition.
Lymph Nodes
- Cancerous Nodes: Typically non-tender.
- Tender Nodes: Often indicate infection.
Mouth
- Gum Issues: Redness and swelling may result from gingivitis or medication use (e.g., Dilantin).
- Salivary Glands: Includes the parotid, submandibular, and sublingual glands.
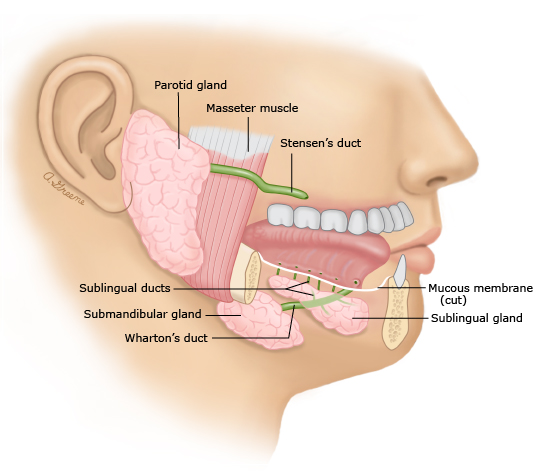
- Sialadenitis: Inflammation of the salivary glands, commonly seen in mumps, causing facial swelling.
- Sialolithiasis (Salivary Stones):
- Presents as a painful lump under the tongue.
- Management: Increased fluid intake, warm compresses, NSAIDs, and antibiotics if infected. Surgery may be necessary for stone removal.
- Torus Palatinus: A painless, bony growth along the midline of the hard palate, usually harmless.
Cheilosis
- Symptoms: Painful cracks and softening at the corners of the mouth.
- Causes:
- Excessive saliva, ill-fitting dentures, nutritional deficiencies, lupus, autoimmune conditions, irritant dermatitis, or squamous cell carcinoma.
- Treatment:
- Address the underlying cause.
- If fungal infection (yeast): Apply azole ointment twice daily.
- If bacterial infection (staph): Use mupirocin ointment twice daily.
- After infection clears: Apply a protective barrier at night, such as:
- Zinc-based creams
- Petroleum jelly
Oral Cancer
- Appearance: Ulcerated lesion with firm, indurated borders.
- Lymph Nodes: Submandibular nodes are often firm and relatively immobile.
- Most Common Type: Squamous cell carcinoma.
- Risk Factors:
- Male gender
- Older age
- Tobacco and alcohol use
- HPV type 16 infection
- Prevention: Routine oral cancer screening during dental visits.
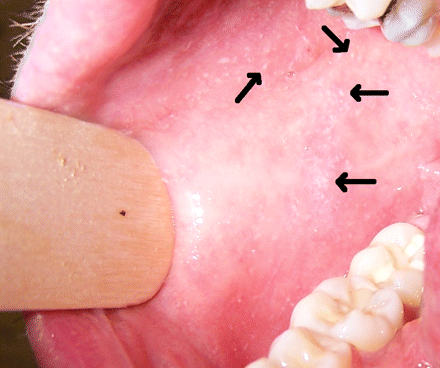
Koplik Spots
- Description: Small red papules with white centers located inside the cheeks, often an early sign of measles.
Red Eye Complaints
Refer to Ophthalmology if the patient presents with:
- Vision changes
- Foreign body sensation preventing eye closure
- Sensitivity to light (photophobia)
Common Symptoms:
- Persistent foreign body sensation
- Scratchy, gritty feeling
- Pink eye (conjunctivitis)
Dacryocystitis
- Cause: Infection of the lacrimal sac/tear duct, typically due to blockage.
- Commonly Affects:
- Infants
- Adults over 40
- Symptoms:
- Thick eye discharge
- Pain, redness, swelling, and warmth of the lower eyelid
- Watery eyes and excessive tearing
- Treatment:
- Gentle lacrimal sac massage (downward motion toward the mouth) 2-3 times daily
- Antibiotic therapy for 7-10 days
Nose
- Nasal Turbinates: Only the inferior turbinates are visible during an exam.
- Allergic Rhinitis Indicators: Pale, swollen, bluish turbinates.
- Sinus Development:
- Frontal sinuses develop around age 5.
- Sphenoid sinuses mature by age 12.
- Rhinitis Medicamentosa:
- Caused by prolonged use of nasal decongestant sprays (longer than 3 days).
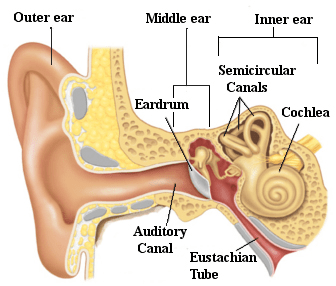
| Hearing Loss Type | Conductive | Sensorineural |
|---|---|---|
| Affected Area | Outer or middle ear | Inner ear |
| Underlying Cause | Obstruction or disruption of sound transmission (e.g., earwax buildup, foreign object, perforated eardrum, serous otitis media, bone abnormality like cholesteatoma) | Damage to the inner ear or auditory nerve (e.g., aging, ototoxic drugs, autoimmune disorders, trauma) |
| Weber Test (Tuning Fork on Forehead) | Sound is louder in the affected ear (e.g., otitis media, impacted cerumen, tympanic membrane perforation) | Sound is louder in the unaffected ear (e.g., presbycusis, Meniere’s disease, nerve damage) |
| Rinne Test (Mastoid Bone → Air Conduction Near Ear) | Negative (Bone conduction > Air conduction) | Normal or positive (Air conduction > Bone conduction) |
| Management | Usually resolves after removing the obstruction, treating infections, or waiting for spontaneous improvement. Rarely requires surgery or medication. Temporary | May require hearing aids or cochlear implants, as it is typically permanent |
Presbycusis: Age-associated decline in hearing ability, particularly challenging in environments with background noise.
Bacterial Causes of Ear Infections
- Streptococcus pneumoniae: Typically results in the most severe symptoms and is least likely to resolve without antibiotics.
- Resistant to low-dose amoxicillin, some cephalosporins, and macrolides.
- Resistance occurs due to modifications in intracellular protein-binding sites.
- High-dose amoxicillin and selected cephalosporins are recommended.
- Risk factor: Recent antibiotic exposure.
- Haemophilus influenzae & Moraxella catarrhalis:
- Gram-negative bacteria capable of producing beta-lactamase.
- Often resolves without treatment.
- H. influenzae is frequently identified in cases of mucoid or serous middle ear infections.
Treatment Guidelines
- No recent antibiotic use:
- High-dose amoxicillin (TID)
- Augmentin (BID)
- Cefdinir
- Recent antibiotic use:
- Augmentin (BID)
- Levofloxacin or Moxifloxacin
Otitis Media with Effusion (OME)
- Managed symptomatically.
- Fluid presence may persist for up to 8 weeks.
Ear Anatomy & Conditions
- Ossicles: Malleus, incus, and stapes.
- Tympanogram: Evaluates middle ear fluid—distinguishes between a flat (fluid-filled) and peaked (normal) response.
- Pinna injuries: Refer to plastic surgery.
- Tragus: Small cartilaginous projection located in front of the ear canal.
- Cerumen buildup (ceruminosis): Can be treated with carbamide peroxide.
HEENT Emergencies
| Condition | Underlying Cause | Symptoms & Indicators | Diagnostic Methods | Recommended Treatment | Key Concerns |
|---|---|---|---|---|---|
| Herpes keratitis | Infection by herpes simplex virus (HSV) or varicella-zoster virus (VZV) | Sudden onset of intense eye pain, sensitivity to light, excessive tearing, and blurred vision, typically affecting one eye. In cases of herpes zoster ophthalmicus, painful vesicular rash appears along the ophthalmic branch of the trigeminal nerve (forehead, eyelids, and nose tip), potentially leading to blindness. | Fluorescein dye staining reveals characteristic dendritic (fern-like) lesions on the cornea, differentiating it from irregular corneal abrasions. | Immediate referral to the emergency department. | Can cause irreversible corneal damage, leading to permanent vision loss. |
| Acute angle-closure glaucoma | Sudden obstruction of aqueous humor drainage, increasing intraocular pressure | Older adults may experience abrupt onset of severe ocular pain, redness, blurred vision, halos around lights, nausea, vomiting, and headache. The pain is caused by the narrowing of the eye’s drainage angle. | The pupil appears mid-dilated and oval-shaped. The cornea looks hazy. Fundoscopic exam reveals cupping of the optic nerve. | Urgent evaluation and treatment in an emergency setting. | A medical emergency; the second leading cause of blindness. High-risk groups include individuals of Asian descent, females, and those who are hyperopic (farsighted). |
| Optic neuritis | Often linked to multiple sclerosis (MS) | Typically affects young women, causing episodes of visual loss in one eye, sometimes accompanied by abnormal eye movements, nystagmus, or neurological symptoms like tingling, muscle weakness, speech difficulties, and unsteady gait. Symptoms worsen with heat and fatigue. | Referral to a neurologist for further evaluation and management. | ||
| Orbital cellulitis | Bacterial infection affecting the tissues around the eye | Rapid onset of a swollen, red eyelid with eye pain, bulging of the eyeball (proptosis), and restricted or painful eye movements. Commonly follows sinus infections or upper respiratory illnesses. | Immediate emergency referral for intravenous antibiotics and possible surgical drainage. | Frequently seen in children and can lead to severe complications, including vision loss and intracranial spread if untreated. | |
| Retinal detachment | Associated with risk factors such as severe myopia, previous eye surgeries (e.g., cataract removal), diabetic retinopathy, aging, or trauma | Sudden appearance of numerous floaters, flashes of light (photopsia), and a shadow or “curtain” obscuring part of the visual field. Distorted or wavy vision may also be reported. | Emergency intervention is required—immediate referral for surgical repair. | ||
| Cholesteatoma | Abnormal growth of keratinizing squamous epithelium in the middle ear | Progressive hearing loss in one ear, foul-smelling ear discharge, and the presence of a mass obstructing the ear canal. Chronic infections may have contributed to its formation. If left untreated, the mass can erode bones and damage the facial nerve (cranial nerve VII). | Referral to an ENT specialist. Treatment includes antibiotics and surgical removal of the lesion. |
HEENT Emergencies Continued
| Condition | Underlying Cause | Symptoms & Indicators | Diagnostic Approach | Recommended Treatment | Key Considerations |
|---|---|---|---|---|---|
| Battle sign | Head trauma | Dark bruising around the eyes (“raccoon eyes”) and behind the ear (mastoid region), typically appearing 2-3 days post-injury. Look for clear, golden fluid leaking from the nose or ear. | Evaluate for possible basilar or temporal bone skull fracture. | Immediate referral to the emergency department (ED). | |
| Clear fluid leakage from nose/ear | Possible basilar skull fracture | Presence of clear, watery fluid draining from the nose or ear, suggesting cerebrospinal fluid (CSF) leakage. | Test the fluid using a urine dipstick—CSF will test positive for glucose, while mucus or pus will not. | Urgent referral to ED. | |
| Peritonsillar abscess | Severe sore throat, difficulty swallowing, painful swallowing (odynophagia), and a distinctive “hot potato” voice. The affected side of the throat appears swollen, pushing the uvula to the opposite side. Symptoms include fever, chills, and general malaise. | Immediate ED referral for drainage and IV antibiotics. | |||
| Diphtheria | Sore throat, fever, and significantly enlarged neck (“bull neck”). Low-grade fever, hoarseness, and difficulty swallowing. A thick, grayish-yellow pseudomembrane covers the throat, tonsils, uvula, and soft palate and is difficult to remove. Highly contagious; requires contact precautions. | Emergency ED referral for diphtheria antitoxin and antibiotics. | |||
| Epiglottitis | Rapid onset of severe sore throat, fever, muffled voice, drooling, difficulty breathing, stridor, and hoarseness. The “thumb sign” may be seen on a lateral neck X-ray. | Urgent referral to ED for airway management and IV antibiotics. | Cases have decreased due to the Hib vaccine but can still occur in unvaccinated individuals. |
HEENT
| Condition | Cause | Symptoms | Diagnosis | Treatment | Additional Considerations |
|---|---|---|---|---|---|
| Corneal Abrasion | Surface injury to the cornea | Sudden onset of intense eye pain, excessive tearing, and sensation of a foreign body. Always check for contact lens use. | Fluorescein dye test reveals a linear or circular defect. | Irrigate with sterile saline, flip the eyelid to inspect for debris. Apply topical antibiotics (e.g., Trimethoprim-Polymyxin B, Ciprofloxacin, Ofloxacin) for 3-5 days. Do not cover the eye. | Complication: Risk of contact lens-related keratitis, characterized by redness, blurred vision, photophobia, and discomfort. |
| Hordeolum (Stye) | Bacterial infection of an eyelash follicle or sebaceous gland. Internal: Involves the meibomian gland. | Rapid development of a painful, red, swollen bump on the eyelid. May rupture and discharge pus. | Apply warm compresses for 5-10 minutes, 2-3 times daily, until it drains. If necessary, prescribe Dicloxacillin or Erythromycin PO four times daily. | Risk: If untreated, may lead to eyelid cellulitis. | |
| Chalazion | Blockage and chronic inflammation of the meibomian gland. | Gradual appearance of a firm, painless, movable lump on the eyelid. If large, it may distort vision by pressing on the cornea. | Options include incision and drainage, surgical excision, or corticosteroid injections. | ||
| Pinguecula | Prolonged exposure to sunlight and UV radiation. | Small, yellowish, raised growth on the conjunctiva near the cornea. | If inflammation occurs, refer to an ophthalmologist for short-term steroid eye drops. Use artificial tears as needed. Preventative: Wear UV-blocking sunglasses. Surgical removal if vision is impaired. | ||
| Pterygium | Chronic sun exposure and irritation. | Thick, wedge-shaped tissue growth on the conjunctiva extending toward the cornea, often on the nasal side. Can become red and irritated. | If inflammation occurs, refer to an ophthalmologist for short-term steroid eye drops. Use artificial tears as needed. Preventative: Wear UV-blocking sunglasses. Surgical removal if vision is impaired. | ||
| Subconjunctival Hemorrhage | Sudden increase in pressure (e.g., coughing, sneezing, heavy lifting, vomiting, minor trauma). | Bright red patch on the sclera due to ruptured blood vessels. Usually painless and does not affect vision. | No treatment needed—resolves on its own within 1-2 weeks. Reassure the patient. | ||
| Primary Open-Angle Glaucoma | Increased intraocular pressure (IOP) due to impaired drainage of aqueous humor. Risk factors: Age, African descent, Type 2 diabetes, family history. | Often asymptomatic in early stages. Gradual loss of peripheral vision leading to tunnel vision. Some patients may notice missing portions of text while reading. Optic disc cupping indicates high IOP. | Refer to an ophthalmologist. Medications: Betimol 0.5% (beta/alpha blocker) to reduce aqueous humor production; Latanoprost (prostaglandin analog). Contraindications: Asthma, COPD, heart failure. | Leading cause of blindness due to optic nerve damage. Risk factors: Postural hypotension, history of fungal eye infections, Caucasian race. | |
| Macular Degeneration | Gradual deterioration of the macula, leading to vision impairment. | Initially symptom-free. Later, central vision loss in one or both eyes, often painless. Straight lines may appear distorted or wavy (scotoma). More prevalent in smokers. | Refer to an ophthalmologist. Patients use an Amsler grid to self-monitor vision weekly. Two types: Dry (atrophic) and Wet (exudative, accounts for 80% of severe cases). | Most common cause of vision loss in older adults. Primary risk factors: Aging, smoking. | |
| Sjogren’s Syndrome | Autoimmune disease affecting moisture-producing glands. | Chronic dryness in the eyes and mouth (xerostomia) lasting over three months. Gritty or sandy eye sensation. Frequent use of artificial tears. | Treat with over-the-counter tear substitutes three times daily. Refer to specialists (ophthalmologist, dentist, rheumatologist) for further care. |
| Condition | Cause | Symptoms | Diagnosis | Treatment | Notes |
|---|---|---|---|---|---|
| Blepharitis | Inflammation of the eyelids, linked to seborrheic dermatitis and rosacea. | Eyelid irritation, itching, redness, a gritty sensation, crusting at lash base. | Lid hygiene with baby shampoo diluted in warm water, erythromycin eye drops (2-3x/day), warm compresses (2-4x/day). | Often associated with seborrheic dermatitis, worsens in winter, may respond to antifungal treatments. | |
| Allergic Conjunctivitis | IgE-mediated allergic reaction. | Itchy, watery, red eyes, yellow rope-like discharge, eyelid swelling, chemosis. | Cool compresses, artificial tears, antihistamine eye drops, mast cell stabilizers, oral antihistamines. | Some medications may cause temporary stinging. | |
| Bacterial Conjunctivitis | Commonly caused by Pseudomonas aeruginosa. | Red eyes, sticky discharge, eyelids stuck together, inflamed conjunctiva. | Polymyxin B/trimethoprim drops, levofloxacin, azithromycin. | Viral conjunctivitis, often caused by adenovirus, should be ruled out. | |
| Allergic Rhinitis | IgE-mediated reaction due to environmental allergens. | Nasal congestion, itching, sneezing, postnasal drip, watery eyes, worsens when lying down. | Nasal examination: Pale, swollen turbinates, clear mucus, cobblestoning in the throat. | Avoid allergens, intranasal corticosteroids (1st-line), antihistamines, decongestants, mast cell stabilizers. | First-generation antihistamines cause drowsiness and should be avoided in some cases. |
| Epistaxis (Nosebleed) | Trauma, medications (NSAIDs, anticoagulants), hypertension, cocaine use. | Sudden-onset nasal bleeding, may vomit blood if swallowed. | Clinical evaluation. | Apply direct pressure, use nasal decongestants (Afrin), cauterize with silver nitrate if needed, petroleum jelly application. | Anterior bleeds (Kiesselbach’s plexus) are milder; posterior bleeds (sphenopalatine artery) can be severe. |
| Strep Throat | Streptococcus pyogenes (Group A Strep), incubation 3-5 days. | Sudden sore throat, fever, headache, swollen cervical lymph nodes, tonsillar exudate, palatal petechiae. | Rapid strep test, throat culture, CENTOR criteria. | Penicillin V, amoxicillin, azithromycin for penicillin allergy, supportive care (hydration, lozenges, pain relievers). | Viral pharyngitis presents with cough, runny nose. Complications include rheumatic fever, post-strep glomerulonephritis. |
| Acute Otitis Media (AOM) | Caused by Strep pneumoniae, H. influenzae, M. catarrhalis. | Ear pain, muffled hearing, recent cold or allergy, bulging red eardrum. | Otoscopic exam: Bulging TM, decreased mobility. | Watchful waiting if mild; amoxicillin (1st-line), Augmentin or cefdinir if prior antibiotics used. | If untreated, may lead to hearing loss, TM rupture, or mastoiditis. |
| Acute Rhinosinusitis | Viral (most cases) or bacterial (Strep pneumoniae, H. influenzae, M. catarrhalis). | Facial pain, upper molar pain, purulent nasal drainage, congestion, sore throat, cough. | Symptoms >10 days, fever >3-4 days, double-worsening pattern. | Symptomatic relief: Saline irrigation, corticosteroids, decongestants; Augmentin for bacterial cases. | Antibiotics only for bacterial cases; avoid macrolides due to resistance. |
| Condition | Cause | Symptoms & Signs | Diagnostic Methods | Treatment Options | Key Considerations |
|---|---|---|---|---|---|
| Otitis Externa | Pseudomonas aeruginosa, S. aureus, Proteus spp., Enterobacteriaceae | Pain, swelling, itching, discharge, and hearing impairment in the outer ear. Recent water exposure (e.g., swimming). Pain when touching the outer ear or tragus. Greenish purulent discharge. Red, inflamed ear canal. | Clinical evaluation. If severe, imaging such as CT, radionucleotide bone scan, gallium scan, or MRI may be needed. | Corticosporin Otic (polymyxin B-neomycin-hydrocortisone) 4 drops, 4x daily for 7 days; Ofloxacin or Ciprofloxacin otic drops twice daily for a week. Keep ears dry. (Avoid steroids if eardrum is perforated.) | Prevention: Use Domeboro (boric acid) or a vinegar-alcohol solution. |
| Mononucleosis | Epstein-Barr Virus (EBV) (incubation: 30-50 days) | Fatigue, fever, sore throat, swollen lymph nodes. History of persistent fatigue and posterior cervical lymph node enlargement. May include abdominal discomfort. Transmitted via saliva. Splenomegaly in 50% of cases. | Bloodwork: Atypical lymphocytosis on CBC; Elevated liver enzymes; Monospot (Heterophile antibody test) positive. Physical exam: Swollen lymph nodes, red throat with possible white exudate, enlarged spleen or liver, red rash. | Avoid strenuous activities for 4 weeks. If spleen/liver enlarged, repeat ultrasound in 4-6 weeks. No amoxicillin. Avoid sharing utensils, kissing, close contact. If breathing difficulty arises, hospitalization and high-dose steroids may be required. | Most common in ages 15-24. Classic signs: “3 F’s and an L” – Fever, Fatigue, Pharyngitis, and Lymphadenopathy. |
| Aphthous Stomatitis | Unknown | Painful, shallow ulcers in the soft tissue of the mouth, resolving in 7-10 days. Commonly known as canker sores. | “Magic mouthwash” (mix of liquid diphenhydramine, viscous lidocaine, and corticosteroids). | ||
| Geographic Tongue | Benign anatomical variation | Irregular smooth patches and fissures on the tongue resembling a topographical map. May cause mild discomfort with acidic or spicy foods. | |||
| Leukoplakia | Ill-fitting dentures, tobacco use, excessive alcohol consumption | Slowly developing white patches with a firm, slightly elevated texture on the tongue, inner cheek, or floor of the mouth. | Precancerous condition. | Referral to a specialist. | |
| Meniere’s Disease | Increased fluid pressure in the inner ear | Recurrent vertigo episodes with a spinning sensation, often preceded by hearing loss, tinnitus, and a feeling of ear fullness. Episodes last from minutes to hours and may be triggered by diet, stress, or hormonal changes. | Diagnosis of exclusion. Horizontal nystagmus (toward affected ear, corrects rapidly). Weber test lateralizes to unaffected ear; Rinne test AC > BC. Symptoms may be triggered by pneumatic otoscopy. Positive Romberg and Fukuda marching tests (drift toward affected side). Dix-Hallpike test occasionally positive (suggests BPPV). | Meclizine (antihistamine), benzodiazepines, or antiemetics for symptom relief. Thiazide diuretics help reduce fluid buildup and prevent future episodes. Corticosteroids may provide relief. Prevention: Minimize sodium intake, avoid loud noises, and steer clear of ototoxic medications. | Risk factors: Long-term exposure to loud noise, prolonged use of ototoxic drugs (e.g., aminoglycosides, high-dose salicylates, chemotherapy drugs). Certain conditions may mimic Meniere’s but are not the disease itself. |