Summary of Key Formulas and Concepts
Cardiac Output (CO)
- Definition: Measures the efficiency of the heart by calculating the amount of blood each ventricle pumps per minute.
- STROKE VOLUME (SV): The amount of blood ejected by each ventricle per heartbeat.
- Formula: CO = SV x HR
- Normal Range: 4-8 L/min
Cardiac Index
- Adjusts cardiac output based on body size (using BMI).
- Normal Range: 2.8-4.2 L/min/m²
Factors that Influence Cardiac Output
- Preload: The degree of stretch in the heart muscle before contraction. Greater stretch leads to stronger contraction.
- Contractility: The strength of heart muscle contractions, which can be enhanced by hormones like norepinephrine and epinephrine.
- Afterload: The resistance the left ventricle must overcome to circulate blood.
Pulse Pressure (PP)
- Definition: The difference between systolic and diastolic blood pressure (PP = SBP – DBP).
- Increased PP: Can be seen with exercise, elevated SBP, arterial stiffness, or early septic shock.
- Decreased PP: May indicate heart failure, low blood volume, or hypovolemic shock.
Ejection Fraction (EF)
- Definition: The percentage of blood the left ventricle pumps out with each contraction.
- Normal Range: 55-70%
Mean Arterial Pressure (MAP)
- Formula: MAP = [SBP + (2 x DBP)] / 3
- Provides an average blood pressure in a cardiac cycle.
Acute Coronary Syndrome (ACS)
Three types of ACS:
- Unstable Angina
- Non-ST-Elevation Myocardial Infarction (NSTEMI)
- ST-Elevation Myocardial Infarction (STEMI)
Indications of Possible ACS
- Chest pain at rest (typically lasting over 20 minutes)
- NEW angina that limits daily activities
- Worsening angina (occurs more often, lasts longer, or is triggered by less exertion)
- Note: Women may have less typical symptoms compared to men.
For cardiac and respiratory arrest – Be familiar with the current AHA ACLS guidelines!
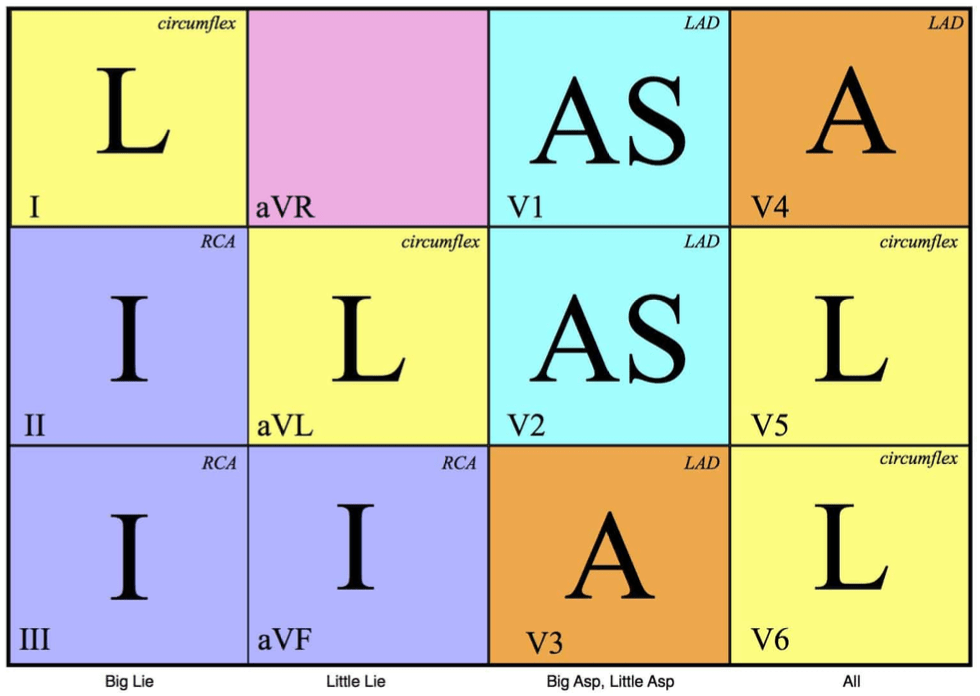
Keep in mind: Major Lie (LII), Minor Lie (LI), SSA (reversed), Everything
EKG Observations
Anterior MI
- Leads: V1, V2, V3, V4
- Affected Artery: Left anterior descending
- Clinical Note: Possible left ventricular failure
Lateral MI
- Leads: I, aVL, V5, V6
- Affected Artery: Circumflex
Posterior MI
- Leads: Reciprocal V3, V2
- Affected Artery: Right coronary artery
- Possible Complications: Bradycardia, heart blocks
- Additional Testing: Requires posterior leads V7, V8, V9
Inferior MI
- Leads: I, III, aVF
- Affected Artery: Right coronary artery
- Complications: Bradycardia, heart blocks
Right Ventricular MI
- Leads: V4R – V6R
- Affected Artery: Right coronary artery
- Complications: Possible right ventricular failure
- Notes: Often occurs with inferior MI. Use right-sided leads if suspected.
LBBB or V-paced rhythm:
In patients with LBBB or V-paced rhythm, identifying an MI can be challenging because abnormal depolarization typically leads to abnormal repolarization, known as appropriate discordance (up and down patterns).
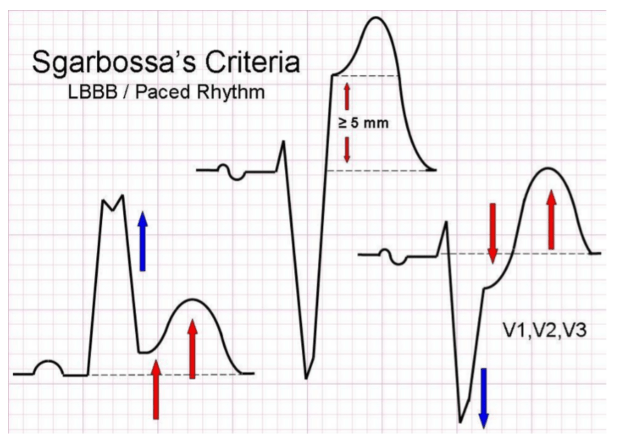
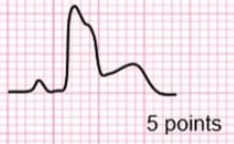
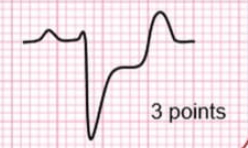
Smith-Modified Sgarbossa Criteria:
1. ST elevation ≥ 1 mm in at least one lead that aligns with the QRS complex (up, up, up).
2. ST depression ≥ 1 mm in at least one lead of V1-V3 that follows the direction of the QRS complex (down, up, up).
3. Excessive discordant ST elevation in at least one lead, where the ST elevation is 25% or more of the depth of the preceding S-wave.
Hs:
- Hypovolemia – Low blood volume, often due to bleeding or severe dehydration.
- Hypoxia – Lack of oxygen.
- Hydrogen ions (Acidosis) – Imbalance in blood pH, typically metabolic acidosis.
- Hyperkalemia or Hypokalemia – High or low potassium levels, affecting heart rhythm.
- Hypothermia – Critically low body temperature.
- Hypoglycemia (less commonly included) – Low blood sugar.
Ts:
- Tension pneumothorax – Collapsed lung due to trapped air causing pressure on the heart.
- Tamponade (cardiac) – Fluid accumulation around the heart, restricting its ability to pump.
- Thrombosis (cardiac or pulmonary) – Blood clot in coronary arteries (heart attack) or lungs (pulmonary embolism).
- Toxins – Drug overdose or poisoning.
- Trauma – Physical injury leading to conditions like hemorrhage or organ damage.
Anginas
Stable angina: Predictable chest pain
- ST depression, occurs only with physical activity, sub-sternal discomfort.
Silent angina: Asymptomatic or minimal symptoms, present in up to 80% of patients.
Unstable angina: New onset or pain at rest, or a worsening pattern of angina. It can involve a ruptured plaque.
- When associated with left anterior descending (LAD) coronary artery lesions, it is referred to as Wellen’s syndrome.
- Inverted T-waves, no ST elevation, and absence of Q waves are present.
- EKG changes occur only when the patient is pain-free; stress testing may precipitate an MI.
Nocturnal angina: Occurs during sleep.
Prinzmetal angina: Chest pain at rest due to coronary artery spasm, often in patients with a history of migraines or Raynaud’s disease.
- Treated with nicardipine.
Angina decubitus: Angina that occurs while lying down.
Myocardial Infarction (MI)
STEMI: Immediate reperfusion is needed through percutaneous intervention or fibrinolytics.
NSTEMI: Requires intensive acute drug therapy such as nitroglycerin, plavix, and heparin.
Heart Failure
Risk factors:
- Coronary artery disease (CAD)
- Increasing age
- Hypertension (3x increased risk)
- Diabetes mellitus
- Smoking
- Obesity
- Hyperlipidemia (HLD)
General concept: The “backup” of blood flow occurs behind the failure, affecting different parts of the body depending on which side of the heart is failing.
- Right-sided heart failure: Affects the body’s organs and tissues that drain to the right side of the heart.
- Symptoms:
- Extremity swelling
- Ascites
- Hepatomegaly
- Jugular venous distention (JVD)
- Symptoms:
- Left-sided heart failure: Affects the lungs that drain to the left side of the heart, leading to pulmonary symptoms.
- Symptoms:
- Pulmonary edema
- Orthopnea
- Dyspnea
- Rales/crackles
- Symptoms:
Systolic (output failure)
- The most common form of heart failure.
- The ventricles have trouble pumping blood effectively.
- Leads to a decrease in ejection fraction.
- Causes include:
- Reduced contractility
- Increased afterload
- Cardiomyopathy
- Mechanical issues
Diastolic (input failure)
- There is impaired filling of the heart, which results in a decreased stroke volume.
- Often seen with pulmonary hypertension.
- Ejection fraction typically remains normal.
Cardiomyopathies:
Abnormal structure or function of the heart.
- Primary: Only the heart is affected.
- Secondary: Resulting from another disease process.
Types:
- Dilated
- Hypertrophic
- Restrictive
- Arrhythmogenic
- Takotsubo
Dilated Cardiomyopathy (most common):
- Enlarged heart with dilated ventricles and atria.
- Impaired systolic function.
- Causes:
- Valvular heart disease
- Ischemic heart disease/hypertension
- Infectious myocarditis
- Genetics
- Idiopathic (commonly alcohol-related, either from alcohol or its metabolites, or additives like cobalt).
Clinical Manifestations:
- Arrhythmias: Atrial fibrillation, ventricular dysrhythmias, sinus tachycardia.
- Extra heart sounds: S3, S4, gallops.
- Symptoms: Fatigue, dyspnea, orthopnea, anorexia, dry cough.
Treatment: Enhance conductivity and decrease afterload.
Hypertrophic Cardiomyopathy:
Asymmetric hypertrophy of the myocardium without ventricular dilation (often genetic).
Manifestations:
- Exertional dyspnea, fatigue, angina, syncope.
Treatment: Beta blockers, calcium channel blockers, or surgery.
Restrictive Cardiomyopathy:
Least common, characterized by impaired relaxation of the heart, preventing diastole.
- Causes: Fibrosis, amyloidosis, hemochromatosis, sarcoidosis, radiation.
Manifestations:
- Angina, syncope, fatigue, dyspnea, exercise intolerance.
Treatment: Similar to CHF management.
Takotsubo Cardiomyopathy (“Broken heart syndrome”):
- Stress-induced acute heart failure that mimics a myocardial infarction (MI) of the anterior wall.
- L ventricular apex bulges while the base hypercontracts.
- Higher risk in post-menopausal women.
Treatment: Supportive care.
Myocarditis:
- Primary or secondary condition causing heart muscle weakness.
- Symptoms: CHF, chest pain, palpitations, sudden death (especially in young adults), fever, rash, joint pain (often viral).
Miscellaneous signs and conditions:
- Wolff-Parkinson-White Syndrome: An abnormal electrical pathway between the atria and ventricles.
- Can lead to supraventricular tachycardia (SVT) and changes on an EKG.
- Quincke’s Sign: Pulsations seen in the capillary bed of the nail, often associated with aortic insufficiency.
- Hill’s Sign: A difference of 40-60 mmHg between the brachial and popliteal blood pressures.
- Pacemaker Syndrome: Occurs when there’s desynchronization between the atria and ventricles.
- Symptoms include forgetfulness, dizziness, syncope, difficulty breathing, orthopnea, swelling, and seizures.
- Brugada Syndrome: A genetic condition marked by ST-segment elevation in leads V1-V3, along with syncope and right bundle branch block (RBBB).
- Pulsus Alternans: The alternation between strong and weak heartbeats, suggesting left ventricular systolic dysfunction.
- Bainbridge Reflex: A response to stretching of the right atrium, which leads to tachycardia.
Cushing Response:
Can occur with increased intracranial pressure (ICP)
- Increased pulse pressure
- Slow heart rate (bradycardia)
- Slow breathing rate (bradypnea)
Beck’s Triad
(used to diagnose cardiac tamponade):
- Low blood pressure
- Swollen neck veins
- Distant or muffled heart sounds
- Treatment: Pericardiocentesis, by inserting a needle 1 cm below the left xiphocostal angle
Virchow’s Triad
(risk factors for deep vein thrombosis):
- Increased blood clotting tendency
- Blood pooling or stagnation
- Injury to blood vessel lining
Pericarditis:
Chest pain relieved by sitting forward, worsened when lying down
- Sharp, pleuritic pain that radiates to the left shoulder
- Friction rub (heard when patient leans forward, at the left sternal border during exhalation)
- ST-segment elevation across all leads
- Chest X-ray may show pericardial effusion
- Treatment: NSAIDs and pericardiocentesis
Costochondritis
Inflammation of the cartilage connecting the ribs. Pain intensifies with touch, deep breaths, and coughing. Often follows an upper respiratory infection.
Mitral Valve Prolapse
Non-specific symptoms such as fatigue, anxiety, dizziness, shortness of breath, palpitations, and fainting. Most individuals show no symptoms.
Cocaine Toxicity
Chest pain, rapid heartbeat, stroke, heart attack, heart failure, seizures, and high blood pressure. Symptoms typically begin within 30-90 minutes.
Systemic Lupus Erythematosus (SLE)
Can cause acute or chronic inflammation affecting various tissues, including the heart.
- Increased risk of atherosclerosis
- Sharp chest pain associated with pleuritis
Hypertensive Crisis
Characterized by extremely high blood pressure accompanied by signs of serious damage to vital organs.
- Avoid rapid blood pressure reduction: It’s advised to gradually lower mean arterial pressure by 20-25% within the first hour to prevent insufficient blood flow to organs.
Affected Organs and Associated Complications
- Heart – Acute coronary syndrome, chest pain, new heart murmur, abnormal heart sounds
- Lungs – Fluid buildup in the lungs (pulmonary edema)
- Abdomen – Abdominal bruit, pulsating mass suggesting an aortic aneurysm
- Brain – Headache, dizziness, vision changes, altered mental state, seizures, localized neurological deficits, subarachnoid hemorrhage
- Kidneys – Acute kidney failure, blood in urine, presence of protein in urine
- Eyes – Retinal bleeding, discharge, swelling of the optic disc (papilledema)
- Pregnancy – HELLP syndrome (breakdown of red blood cells, high liver enzymes, low platelet count)
Medications and Mechanism of Actions
- Nitroprusside – Lowers both preload and afterload, acts quickly with a short duration
- Nitroglycerin – Reduces preload and decreases cardiac output
- Labetalol – Blocks both alpha and beta receptors. Not recommended for heart failure, slow heart rate, or reactive airway disease
- Hydralazine – Dilates arteries, commonly preferred for managing preeclampsia
Aortic Dissection
- Sudden sharp, tearing pain that may spread to the back or neck
- Check blood pressure in both arms as a priority. A difference of more than 20 mmHg is significant
Peripheral Artery Disease (PAD) / Peripheral Vascular Disease
- Intermittent claudication: Muscle pain or cramping in the calf that improves with rest
- Caused by narrowing of the arteries due to plaque buildup
- May also experience nighttime foot cramps
6 Signs of Ischemia
- Pain
- Pale skin (Pallor)
- No pulse (Pulselessness)
- Tingling or numbness (Paresthesia)
- Muscle weakness or paralysis
- Cool temperature in the affected area (Poikilothermia)
Buerger’s Disease
- Ongoing inflammation in the small blood vessels of arms and legs
- Common in young male smokers
- Symptoms include red or bluish skin, no detectable pulse, and thin, shiny skin
Ulcers: Venous vs. Arterial
Causes
- Venous: Deep vein thrombosis (DVT), obesity, faulty valves
- Arterial: Aging, smoking, plaque buildup in arteries, high blood pressure, diabetes
Common Locations
- Venous: Front of lower leg, inner ankle
- Arterial: Toe tips, between toes, over joints of toes, outer ankle, bottom of foot
Pain Level
- Venous: Mild to moderate discomfort, relieved by raising the leg
- Arterial: Severe pain, eased by lowering the leg
Skin Characteristics
- Venous: Swollen, softened skin, warm, flaky, reddish-brown color, normal hair and pulses
- Arterial: Thin, shiny skin, thickened nails, cold to touch, hair loss, weakened pulses
Ulcer Description
- Venous: Irregular borders, no dead tissue, red base
- Arterial: Clear, defined edges, dead tissue present, pale center
Infective Endocarditis
General Symptoms: Fever, tiredness, loss of appetite, weight loss
Osler’s Nodes: Painful, red bumps on fingers and toes.
Memory Tip: “Dr. Osler is a pain, always snapping his fingers and tapping his feet.”
Janeway Lesions: Painless, small red or bleeding spots on palms or soles. Only a few millimeters in size.
Memory Tip: “Jane is so small and gentle, she wouldn’t cause any pain.”
Roth’s Spots: Retinal hemorrhages with pale centers
IO Insertion Procedure
- Locate the correct anatomical site
- Disinfect the area
- Attach the proper needle to the drill and remove the safety cap
- Insert the needle through the skin until it touches the bone
- Drill the needle straight into the bone using steady pressure
- Ensure about 5 mm of the catheter remains visible above the skin; if not, a longer needle may be needed
- Continue drilling until a “give” or “pop” is felt, indicating entry into the medullary space
- Carefully remove the stylet (it is very sharp—dispose of it in a sharps container)
- Connect the extension set provided by the manufacturer (pre-flushing with saline or lidocaine can be useful)
- Confirm correct placement by drawing back blood or marrow (should appear reddish and frothy)
- If the patient is conscious, administer 2-3 mL of 2% lidocaine slowly (to minimize pain from cavity expansion)
- Flush saline through the extension set to expand the marrow cavity, ensuring good flow rates
- Secure the IO line with an appropriate dressing