Heart Murmurs
- Result from turbulent blood flow through major vessels or heart valves.
- Classified by timing (systolic vs. diastolic) and location (aortic vs. mitral).
Systolic Murmurs – “MR Peyton Manning AS MVP”
- Mitral Regurgitation – Holosystolic (pan-systolic) murmur.
- Location: Best heard at the apex of the heart.
- Radiation: Extends to the axilla.
- Sound: High-pitched, blowing murmur.
- Best Heard With: Diaphragm of stethoscope.
- Physiologic Murmur – Occurs due to temporary conditions like severe anemia or dehydration.
- Louder when lying down.
- Aortic Stenosis – Harsh, noisy murmur.
- Location: 2nd intercostal space (ICS), right of sternum.
- Radiation: Extends to the neck.
- Considerations:
- Increased risk of sudden cardiac death—avoid strenuous activity.
- Monitored via echocardiogram; may require valve replacement.
- Common causes: Congenital defect (in children), previous rheumatic fever.
- Symptoms: Chest pain (angina), fainting (syncope), heart failure.
- Mitral Valve Prolapse (MVP) – Mid-to-late systolic murmur with a mid-systolic click.
Diastolic Murmurs – “ARMS”
- Aortic Regurgitation – High-pitched blowing murmur.
- Location: 2nd ICS, right of sternum.
- Best Heard With: Diaphragm.
- Mitral Stenosis – Low-pitched murmur.
- Location: Apex (apical area).
- Also Called: “Opening snap,” “crescendo murmur”.
- Best Heard With: Bell of the stethoscope.
Key Point: All diastolic murmurs are abnormal.
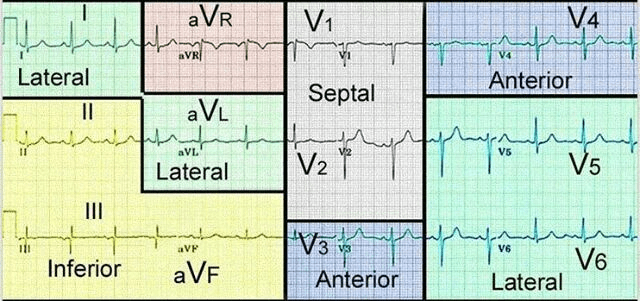
Valve Locations (APETM)
- Aortic Valve – 2nd ICS, right upper sternal border.
- Pulmonic Valve – 2nd ICS, left upper sternal border.
- Erb’s Point – 3rd ICS, left of sternum (often used for S2 sounds).
- Tricuspid Valve – 4th ICS, left lower sternal border.
- Mitral Valve – 5th ICS, left midclavicular line (PMI or apical area).
Murmur Radiation
- Axilla: Likely a mitral valve issue.
- Neck: Likely an aortic valve issue.
Valve Dysfunction
- Stenotic valves fail to open properly.
- Incompetent (regurgitant) valves fail to close properly.
Murmur Grading Scale
- Grade I/VI – Very faint, barely audible.
- Grade II/VI – Clearly audible but soft.
- Grade III/VI – Moderate volume, as loud as S1.
- Grade IV/VI – Loud, often accompanied by a palpable thrill.
- Grade V/VI – Very loud, heard with the stethoscope partially lifted off the chest.
- Grade VI/VI – Loudest, can be heard even without a stethoscope.
Using a Stethoscope
- Bell – Best for low-pitched sounds (S3, S4, mitral stenosis).
- Diaphragm – Best for mid-to-high pitch sounds (lung sounds, mitral regurgitation, aortic stenosis).
Heart Sounds
Mnemonic: “Motivated Apples”
- S1 (“lub”) – Occurs during systole (AV valve closure).
- M – Mitral valve.
- T – Tricuspid valve.
- AV – Atrioventricular valves.
- S2 (“dub”) – Occurs during diastole (semilunar valve closure).
- A – Aortic valve.
- P – Pulmonic valve.
- S – Semilunar valves.
Additional Heart Sounds
- S3 (“ventricular gallop”) – Suggests congestive heart failure (CHF) in patients >35 years old.
- Can be normal in adolescents, pregnancy, and thyrotoxicosis.
- Sounds like “Kentucky”; best heard at pulmonic area.
- S4 (“atrial gallop”) – Indicates left ventricular hypertrophy (LVH), uncontrolled hypertension, or unstable angina.
- Common in elderly patients.
- Sounds like “Tennessee”; best heard at apex with the bell.
- Split S2 – Heard best at the pulmonic area, normal in young athletes.
Fibrinolysis Contraindications
Absolute Contraindications (High Risk – Avoid Use)
- History of intracranial hemorrhage (previous brain bleed).
- Cerebral vascular abnormalities (aneurysms, arteriovenous malformations).
- Brain tumors (primary or metastatic).
- Ischemic stroke within the past 3 months.
- Suspected aortic dissection.
- Active internal bleeding (excluding menses).
- Recent intracranial or intraspinal surgery (within 2 months).
- Severe, uncontrolled hypertension (posing a risk of hemorrhage).
Relative Contraindications (Consider Risks vs. Benefits)
- Chronic uncontrolled hypertension or marked hypertension upon presentation.
- Recent ischemic stroke (< 3 months ago).
- Prolonged or traumatic CPR.
- Major surgery within the past 3 weeks.
- Recent internal bleeding (within 2-4 weeks).
- Non-compressible vascular punctures (e.g., subclavian or jugular vein access).
- Pregnancy.
- Active peptic ulcer disease.
- Current use of oral anticoagulants (warfarin, DOACs).
Key Cardiovascular Concepts
- Blood Pressure Formula:
BP = HR x SV x PVR- HR – Heart Rate
- SV – Stroke Volume
- PVR – Peripheral Vascular Resistance
- Left vs. Right Heart Pressures:
- Left side of the heart operates at higher pressures (arterial system).
- Right side of the heart functions at lower pressures (venous system).
- Most abnormalities originate from left-sided heart disease.
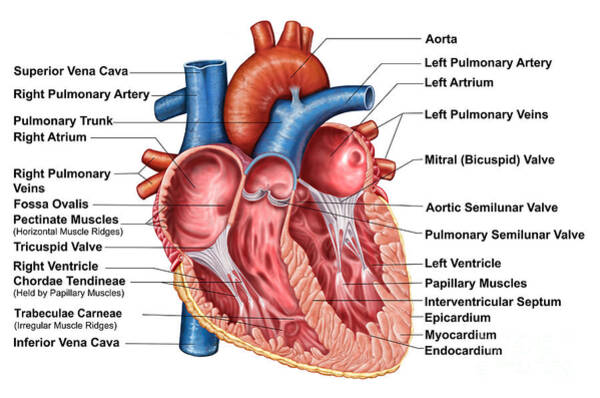
- Blood Flow Through the Heart:
Deoxygenated Blood Pathway:
Superior vena cava → Right atrium → Tricuspid valve → Right ventricle → Pulmonary valve → Pulmonary arteries → Lungs
(RBCs exchange CO2 for O2 in alveoli)Oxygenated Blood Pathway:
Pulmonary veins → Left atrium → Mitral valve → Left ventricle → Aortic valve → Systemic circulation
Hypertrophy & Cardiac Changes
- Left Ventricle: Most likely chamber to hypertrophy.
- Common in hypertension (HTN) target organ damage (TOD).
- PMI shifts downward & laterally in left ventricular hypertrophy (LVH).
- Normal PMI location: 5th ICS, midclavicular line (MCL).
- Left Atrium: Second most common chamber to hypertrophy.
- Aortic Stenosis:
- Most common pathological murmur associated with aging.
- Mitral Regurgitation (MR):
- Most common regurgitant murmur (caused by mitral valve failing to close properly).
- Leads to reduced cardiac output.
Signs of Low Cardiac Output
- Dyspnea on exertion (shortness of breath with activity).
- Chest pain.
- Orthopnea (shortness of breath when lying flat; often indicates heart failure rather than lung disease).
- Syncope or near-syncope (often due to aortic stenosis or hypertrophic obstructive cardiomyopathy).
Hypertrophic Obstructive Cardiomyopathy (HOCM)
- Genetic condition (autosomal dominant inheritance).
- Also known as idiopathic hypertrophic subaortic stenosis.
Mitral Regurgitation (MR) – Clinical Exam Findings
- Murmur Characteristics:
- Holosystolic murmur (persists throughout systole with consistent intensity).
- Blowing quality (soft or whooshing sound).
- Grade II-III/IV murmur.
- Radiates to the axilla.
Assessing Unexpected Cardiac Findings
- If a sudden, unexpected murmur or symptom is discovered, ask:
- Onset – When did it begin?
- Location & Radiation – Where is it heard, and does it spread elsewhere?
- Duration – How long has it been present?
- Character – What does it sound like?
- Aggravating Factors – What makes it worse?
- Relieving Factors – What improves it?
- Timing – When does it occur (rest vs. exertion)?
- Severity – How intense is it?
Target Organ Damage in Hypertension
- Eyes: Hypertensive retinopathy, increasing the risk of blindness.
- Findings: Silver or copper wiring of arterioles, AV nicking, flame-shaped hemorrhages (appearing as black spots in vision), and papilledema.
- Kidneys: Signs of renal damage include:
- Microalbuminuria & proteinuria
- Elevated creatinine & decreased GFR
- Edema due to fluid retention
- Cardiovascular System:
- S3 heart sound (congestive heart failure)
- S4 heart sound (left ventricular hypertrophy)
- Carotid bruits (suggesting atherosclerosis)
- Conditions: CAD, MI, LVH, PAD/PVD
- Brain: Increased risk of TIA (transient ischemic attack) & stroke (CVA).
Lifestyle Modifications for Hypertension & Dyslipidemia
- Quit smoking & reduce stress levels.
- Weight loss (if overweight/obese):
- 5–20 mmHg reduction per 10 kg lost.
- DASH diet:
- Increase fruits, vegetables, potassium, and calcium.
- Reduce sodium intake.
- Consume fatty cold-water fish at least 3 times per week.
- Sodium intake: Limit to <2.4 g/day.
- Exercise:
- Aerobic activity (40 minutes, 3-4 days per week).
- Alcohol moderation:
- Men: <2 drinks/day
- Women: <1 drink/day
Aldosterone Antagonist Diuretics
Mechanism of Action:
Blocks the effects of aldosterone, promoting sodium and water excretion while conserving potassium. Also exhibits anti-androgenic effects.
Indications:
- Hypertension (HTN)
- Congestive Heart Failure (CHF)
- Hirsutism and precocious puberty (off-label use due to anti-androgenic activity)
Common Side Effects:
- Gynecomastia (more common with spironolactone)
- Hyperkalemia
Contraindications:
Avoid use in combination with:
- Other potassium-sparing diuretics
- ACE inhibitors (ACEIs) or potassium supplements
- Renal insufficiency
- Diabetes with microalbuminuria (increased risk of hyperkalemia)
Examples:
- Spironolactone (Aldactone)
- Eplerenone (Inspra)
JNC-8 Hypertension Guidelines
While JNC 8 previously recommended a target of <150/90 mmHg for adults ≥60, more recent guidelines from the ACC/AHA 2017 now define:
Blood Pressure Categories:
- Normal: <120/80 mmHg
- Elevated: 120–129/<80 mmHg
- Stage 1 Hypertension: 130–139/80–89 mmHg
- Stage 2 Hypertension: ≥140/90 mmHg
Treatment Goals:
- Most adults, including healthy older adults: Target <130/80 mmHg
- Consider individualized targets in frail or high-risk elderly patients
First-Line Antihypertensive Medications:
- Non-Black adults: Thiazide diuretics, ACE inhibitors (ACEIs), angiotensin receptor blockers (ARBs), or calcium channel blockers (CCBs) — used alone or in combination
- Black adults: Thiazide diuretics or CCBs — alone or in combination
- Chronic Kidney Disease (CKD): ACEI or ARB preferred, alone or with other agents
Treatment Strategy:
- Begin with lifestyle modifications for all patients
- Initiate medication based on BP level and cardiovascular risk
- Maximize first drug dose or add a second agent from a different class if needed
- Consider combination therapy upfront for Stage 2 HTN or significantly elevated BP
Note: While JNC 8 can be referenced historically, the <130/80 mmHg goal is now the standard target for most patients according to ACC/AHA guidelines.
Thiazide Diuretics
- MOA: Reduces blood volume, venous pressure, and preload.
- Most effective in Black patients.
- May cause erectile dysfunction (ED).
- Beneficial in osteoporosis:
- Calcium-sparing effect lowers fracture risk.
- High doses (>25 mg/day) increase risks:
- Hyperglycemia, hyperlipidemia, hyperuricemia (gout)
- Monitor: Sodium (Na+), potassium (K+), and magnesium (Mg++) levels.
- Example: Hydrochlorothiazide (HCTZ) – contraindicated in sulfa allergy.
Calcium Channel Blockers (CCBs) – “-ipine” Drugs
- MOA: Causes systemic vasodilation and slows heart rate.
- Most potent BP-lowering medication.
- Types:
- Dihydropyridines (DHPs) → Lower BP without affecting HR
- Example: Amlodipine
- Non-Dihydropyridines (Non-DHPs) → Lower BP & HR slightly
- Examples: Diltiazem, Verapamil
- Dihydropyridines (DHPs) → Lower BP without affecting HR
- First-line treatment for Black patients with HTN.
- Side Effects: Headache, ankle edema, bradycardia, reflex tachycardia.
- Contraindications:
- Heart block, bradycardia, CHF.
- Avoid: Grapefruit, macrolide antibiotics.
- More effective when taken at night.
Digoxin
- ECG in therapeutic range: Prolonged PR interval, depressed/cupped ST segment.
- ECG in toxicity: AV heart block.
- Signs of toxicity: Anorexia.
- Drug interactions: Amiodarone, diltiazem, macrolides, antifungals, cyclosporine, verapamil.
Loop Diuretics
- Examples:
- Furosemide (Lasix)
- Bumetanide (Bumex)
- MOA: Inhibits the sodium-potassium-chloride pump in the kidneys, increasing urine output.
- Side Effects:
- Electrolyte imbalances: Hypokalemia, hyponatremia, hypomagnesemia.
Alpha-1 Blockers (“-ozin” Drugs)
- Indications: Benign prostatic hyperplasia (BPH) & hypertension.
- Side Effects: Orthostatic hypotension, dizziness, postural hypotension (especially with the first dose).
- Dosing Strategy: Start low, titrate up, and give at bedtime.
- Examples:
- Terazosin (Hytrin)
- Tamsulosin (Flomax)
- Carvedilol: Acts as both an alpha- and beta-adrenergic antagonist.
Beta-Blockers (“-olol” Drugs)
- MOA: Blocks beta-1 receptors in the heart, reducing heart rate and stroke volume.
- Indications:
- Post-MI, migraines, glaucoma, resting tachycardia, angina, hyperthyroidism.
- Caution:
- May worsen asthma, COPD.
- Contraindicated in heart block, bradycardia.
- Efficacy:
- More effective in White patients for BP control (4th-line antihypertensive).
- Primarily used for heart failure rather than BP control.
- Reduces effects of circulating catecholamines.
ACE Inhibitors (“-pril”) & ARBs (“-sartan”)
- MOA: Blocks the conversion of angiotensin I to angiotensin II.
- First-line choice for:
- Hypertension with diabetes or kidney disease.
- Side Effects:
- Dry hacking cough (more common with ACE inhibitors).
- Hyperkalemia, angioedema.
- Dosing Adjustments: Needed in renal insufficiency.
- Contraindications:
- Pregnancy, renal artery stenosis, acute renal insufficiency.
Dyslipidemia
Screening & Detection
- Lipid profile recommended for individuals with cardiovascular risk factors, including:
- Diabetes mellitus (DM)
- Hypertension (HTN)
- Strong family history of dyslipidemia or early cardiovascular disease
- Obesity
- 12-hour fasting required before testing.
- Key lipid panel components:
- Total cholesterol (TC)
- Low-density lipoprotein (LDL) – “bad” cholesterol
- High-density lipoprotein (HDL) – “good” cholesterol
- Triglycerides (TG)
Dietary Modifications to Lower LDL (5-10% Reduction)
- Increase plant sterols (found in cholesterol-lowering margarine):
- Take Control, Benecol
- Consume fiber-rich foods:
- Oatmeal, oat bran
Reduce Intake of Saturated Fat & Cholesterol
- Avoid trans fats (found in processed and fried foods).
- Keep total cholesterol intake below 200 mg/day.
Increase Omega-3 Fatty Acids for Heart Health
- Eat fatty fish at least twice per week (e.g., salmon, mackerel, sardines).
- Other sources:
- Flaxseed
- Walnuts
- Canola and soybean oils
- For those with coronary heart disease (CHD):
- Consume 1 gram of EPA + DHA daily (via 4 oz salmon daily or fish oil supplements).
Statin Therapy Overview
| Category | High-Intensity | Moderate-Intensity | Low-Intensity |
|---|---|---|---|
| Usage Considerations | Avoid in individuals over 80, those with impaired kidney function, frailty, multiple comorbidities, or when combined with fibrates | Preferred for patients at higher risk of adverse effects | Generally not recommended |
| LDL Reduction | Reduces LDL by approximately ≥50% | Reduces LDL by 30-49% | Reduces LDL by <30% |
| Medications & Dosages | – Atorvastatin 40-80 mg – Rosuvastatin 20-40 mg | – Atorvastatin 10-20 mg – Rosuvastatin 5-10 mg – Simvastatin 20-40 mg – Pravastatin 40-80 mg – Lovastatin 40 mg | – Pravastatin 10-20 mg – Lovastatin 20 mg – Simvastatin 10 mg |
Cholesterol Management: Additional Considerations
Statin therapy is now guided primarily by cardiovascular risk categories rather than specific LDL targets. The focus is on risk-based treatment, as supported by the ACC/AHA, USPSTF, and ADA 2023 guidelines.
When to Use Statins:
- Clinical ASCVD (e.g., prior MI, stroke, or PAD):
→ Recommend high-intensity statin - LDL ≥190 mg/dL (regardless of risk):
→ Recommend high-intensity statin - Diabetes (age 40–75 years):
→ Recommend moderate-intensity statin
→ Consider high-intensity statin if additional risk factors or 10-year ASCVD risk ≥20% - 10-year ASCVD risk ≥7.5% (no ASCVD or diabetes):
→ Recommend moderate- to high-intensity statin, based on shared decision-making - Ages >75:
→ Statin use should be individualized, as evidence is more limited
Key Notes:
- The goal is to reduce overall cardiovascular risk, not necessarily to reach a specific LDL number (e.g., LDL <100 mg/dL is no longer a universal treatment target)
- Diabetic patients aged 40–75 are generally treated with at least moderate-intensity statins, per ADA 2023 guidelines
- Statins are often taken at night, especially shorter-acting ones (e.g., simvastatin), though some newer agents can be taken at any time
- If prescribed, baby aspirin may be used alongside statins for secondary prevention, but not routinely for primary prevention
Weight and Obesity
- Body Mass Index (BMI): Measurement comparing weight and height
- Formula: Weight (kg) ÷ Height (m²)
- May overestimate BMI in muscular individuals
- BMI Categories:
- Underweight: Below 18.5
- Healthy Weight: 18.5 – 24.9
- Overweight: 25 – 29.9
- Obese: 30+
- Waist and Hip Measurements:
- Men: Waist > 40 inches
- Women: Waist > 35 inches
- Waist-to-Hip Ratio: >1.0 (men), >0.8 (women)
- Metabolic Syndrome Diagnosis: Requires three of the following:
- Abdominal obesity (waist circumference)
- High blood pressure
- Abnormal lipid levels (elevated triglycerides, low HDL, insulin resistance)
- Fasting glucose > 100 mg/dL or diabetes diagnosis
Statins (HMG-CoA Reductase Inhibitors)
- Effects on Lipids:
- Reduces LDL by 18–55%
- Increases HDL by 5–15%
- Lowers triglycerides by 7–30%
- Monitoring: Baseline liver enzyme test; no ongoing checks needed
- Cautions: Avoid grapefruit juice with simvastatin, atorvastatin, lovastatin
- Potential Side Effects:
- Rhabdomyolysis, muscle inflammation (myositis)
- Risk Factors for Myositis: Older age, low body weight, high-dose statins
Bile Acid Sequestrants
- Effects on Lipids:
- Decrease LDL by 15–30%
- Slightly raise HDL by 3–5%
- May increase triglycerides if levels exceed 400 mg/dL
- Examples: Cholestyramine, colestipol, colesevelam
- Side Effects: Constipation, reduced absorption of other medications
Niacin (Vitamin B3)
- Effects on Lipids:
- Lowers LDL by 5–25%
- Increases HDL by 15–35%
- Reduces triglycerides by 20–50%
- Side Effects:
- Flushing (can be minimized with aspirin 1 hour before)
- Increased blood sugar, uric acid, digestive discomfort, liver toxicity
Fibrates
- Effects on Lipids:
- Reduces LDL by 5–20%
- Increases HDL by 10–20%
- Decreases triglycerides by 20–50%
- May raise LDL in individuals with very high triglycerides
- Side Effects: Indigestion, gallstones, muscle issues
- Contraindications: Not recommended for severe kidney or liver disease
- Example: Fenofibrate
Omega-3 Fatty Acids (Fish Oil)
- Recommended Dose: 4 grams per day
- Effects on Lipids:
- Lowers triglycerides by 20–30%
- Side Effects:
- Increased bleeding risk
- Gastrointestinal discomfort (fishy aftertaste) – can be reduced by freezing capsules, taking with meals, and avoiding hot drinks immediately after
Causes of Secondary High Triglycerides
- Underlying Conditions:
- Uncontrolled or untreated hypothyroidism
- Poorly managed diabetes
- Excessive alcohol consumption
Cholesterol Absorption Inhibitors
- Effects on Lipids:
- Reduces LDL by 15–20%
- Slightly increases HDL by 3–5%
- Examples: Ezetimibe (Zetia) – often used in combination therapy (e.g., Vytorin)
Cardiovascular System
| Condition | Causes | Signs & Symptoms | Diagnostics | Treatments | Concerns |
|---|---|---|---|---|---|
| Acute Coronary Syndrome (STEMI, NSTEMI, Unstable Angina) | Unstable angina caused by vasoconstriction, non-occlusive thrombus, inflammation, or infection | Central chest pain (squeezing, tightness, crushing pressure), numbness/tingling in left jaw/arm, cold/clammy sweating. Pain triggered by exertion or heavy meals, persists at rest. Women may experience fatigue, sleep disturbances, anxiety, weakness, nausea, dyspnea, syncope, back pain | EKG | Beta-blockers, ACE inhibitors, aldosterone antagonists | STEMI: full-thickness MI with Q waves. NSTEMI: partial occlusion. Stable angina: predictable pain pattern. |
| Congestive Heart Failure (Left-Sided) | MI, CAD, HTN, fluid retention, valvular disease, arrhythmias | Bilateral lung crackles, S3 heart sound, cough, dyspnea, dullness to percussion, nocturnal dyspnea, orthopnea, non-productive cough, wheezing (“left = lung”) | Chest X-ray (Kerley B lines), EKG, troponin, BNP, CMP, echocardiogram | Monitor weight, avoid alcohol, quit smoking, diuretics, ACEI/ARB, beta-blockers (if HFrEF), aldosterone antagonists, sodium restriction (2-3g), fluid restriction (1.5-2L) | Ejection Fraction (EF): HFrEF <40% (systolic failure), HFpEF >40% (diastolic failure). Medications contributing to HF: NSAIDs, amlodipine, metoprolol (still needed), glitazones (Actos/Avandia). NYHA classification: Class I (no limits) – Class IV (symptoms at rest). |
| Congestive Heart Failure (Right-Sided) | MI, CAD, HTN, fluid retention, valvular disease, arrhythmias | Jugular venous distension (>4cm), enlarged spleen/liver causing nausea, anorexia, abdominal pain, lower extremity edema (“right = GI”) | Same as left-sided HF | Same as left-sided HF | Same as left-sided HF |
| Bacterial Endocarditis | Gram-positive bacteria (Viridans streptococcus, Staphylococcus aureus) | Fever, chills, new murmur, sudden CHF. Subungual hemorrhages, petechiae on palate, painful Osler nodes (fingers/toes), non-tender Janeway lesions (palms/soles), Roth spots (retinal hemorrhages), hematuria | Blood cultures (x3), CBC, ESR >20 mm/hr | Refer to cardiology. Prophylaxis: no longer needed for MVP/GU/GI, but required for prior endocarditis, prosthetic valves, congenital heart disease. Antibiotics: Amoxicillin 2g PO (adult) or 50mg/kg (peds) 1 hr pre-procedure. If allergic: Clindamycin 600mg, Biaxin 500mg, Keflex 2g, macrolide alternative | Risks: valve destruction, myocardial abscess, emboli |
| Dissecting Abdominal Aortic Aneurysm | Pulsating abdominal mass, severe sharp back/chest pain, hypotension, distended abdomen | Abdominal ultrasound. CXR may show widened mediastinum, tracheal deviation, obliteration of aortic knob | Surgical repair. If <4cm, monitor annually via CT scan | Risk factors: male >60, smoker, uncontrolled HTN, white race, genetic conditions (Marfan syndrome) | |
| Atrial Fibrillation | HTN, CAD, ACS, caffeine, nicotine, hyperthyroidism, alcohol, HF, LVH, PE, COPD, sleep apnea | May be asymptomatic or present with HR >110 bpm. If unstable: chest pain, hypotension, heart failure, clammy skin, acute kidney injury | 12-lead EKG, TSH, electrolytes, renal function, 24-hour Holter, echocardiogram | Avoid stimulants. Identify underlying cause. Refer to cardiology if CHA₂DS₂-VASc score >2 (anticoagulation needed: Warfarin INR 2-3, for valves 2.5-3.5). HR control: CCB, beta-blockers, digoxin | Most common arrhythmia (SVT class), increases stroke risk. Paroxysmal AF: lasts <7 days. INR >4-5: hold dose, adjust maintenance dose. |
| Paroxysmal Supraventricular Tachycardia (PSVT) | Digitalis toxicity, alcohol, hyperthyroidism, caffeine, stimulant drugs | Sudden onset palpitations, rapid pulse, lightheadedness, dyspnea, anxiety (HR 150-250 bpm) | EKG | Vagal maneuvers, carotid massage, cold water to face. If WPW syndrome or symptomatic: emergency intervention (911) | May occur in Wolff-Parkinson-White syndrome |
Cardiovascular
| Condition | Causes | Signs & Symptoms | Diagnostics | Treatments | Concerns |
|---|---|---|---|---|---|
| Pulsus Paradoxus | Asthma, emphysema, cardiac tamponade, pericarditis, pericardial effusion | Apical pulse remains audible while the radial pulse disappears; detected via stethoscope and BP cuff. Heart chamber compression causes an exaggerated drop in systolic BP (>10 mmHg) | Clinical assessment | Identify and treat underlying condition | Indicates severe cardiac or respiratory dysfunction |
| Hypertension | Changes in peripheral vascular resistance (PVR) or cardiac output (CO) alter BP | Often asymptomatic. Normal: <120/80 mmHg. Prehypertension: 120-139/80-89. Stage 1: 140-159/90-99. Stage 2: ≥160/100. Secondary HTN: Suspect in patients <30 years old, severe HTN, acute BP rise, resistant HTN (on 3 meds). Possible causes: Renal (renal artery stenosis, polycystic kidney disease, CKD), Endocrine (hyperthyroidism, hyperaldosteronism, pheochromocytoma), Other (sleep apnea, aortic coarctation) | Confirm elevated BP on 2 separate visits. BP goals: <140/90 if <60 years old; <150/90 if >60 years old with no comorbidities. Tests: Creatinine, GFR, UA (kidneys), TSH, glucose (endocrine), K+/Na+/Ca2+ (electrolytes), cholesterol, CBC, baseline EKG, CXR | Hypertensive emergency: Diastolic BP >120 with symptoms (N/V, stroke, MI, renal failure, retinopathy, aortic dissection). Treatment: Thiazides, CCBs, ACEI/ARBs | Isolated systolic HTN: SBP >160 due to arterial stiffness and increased PVR. Younger patients have higher renin levels; pregnancy reduces vascular resistance. |
| Deep Vein Thrombosis (DVT) | Blood clot formation due to stasis, trauma, inflammation, or hypercoagulation | Gradual unilateral leg swelling, pain, redness, warmth. If pulmonary embolism (PE): Sudden chest pain, dyspnea, dizziness, syncope | Tests: +Homan’s sign (33% of cases), CBC, platelets, PT/PTT, INR, D-dimer, chest X-ray, EKG, ultrasound | Treatment: Refer to Wells Criteria. Warfarin takes 3-5 days for full effect; maintain INR 2-3. Interactions: Clarithromycin ↑ warfarin effect, cholestyramine ↓ warfarin effect. Consider direct thrombin inhibitors (Pradaxa) | Risk factors: Prolonged immobility (bed rest, long travel), CHF, clotting disorders (Factor V Leiden, protein C deficiency), estrogen use (OCPs, pregnancy), trauma, malignancy |
| Superficial Thrombophlebitis | Inflammation of superficial veins due to trauma or secondary infection (Staphylococcus aureus) | Localized redness, swelling, tenderness, vein feels hardened (indurated). Usually in extremities. Afebrile, normal vitals | Clinical exam: palpable, cord-like, warm, tender vein without edema | NSAIDs, warm compress, elevate limb | Usually self-limiting; treat underlying cause |
| Peripheral Artery Disease (PAD) | Narrowing or occlusion of medium-to-large arteries in the lower extremities (arterial insufficiency) | Leg pain worsens with walking, relieved by rest (claudication – “angina of the legs”). Thin, hairless skin, thickened/discolored toenails, absent dorsalis pedis pulse, possible toe gangrene | Check dorsalis pedis/posterior tibial pulses, ABI <0.9, Doppler ultrasound, refer to vascular specialist | Management: Smoking cessation, daily walking. Medications: Cilostazol (Pletal) with aspirin or Plavix (caution with grapefruit juice, diltiazem, omeprazole); Pentoxifylline (Trental) (limited benefit) | Complications: Foot gangrene, CAD, carotid artery plaque, increased risk with HTN, smoking, diabetes, hyperlipidemia. May lead to osteomyelitis. |
| Raynaud’s Phenomenon | Reversible vasospasm of peripheral arterioles in fingers/toes | Episodic color changes: white (pallor) → blue (cyanosis) → red (reperfusion). Numbness, tingling, episodes lasting hours. Associated with autoimmune diseases (thyroid disorders, pernicious anemia, rheumatoid arthritis). More common in women (8:1), secondary Raynaud’s linked to scleroderma | Check distal pulses | Lifestyle changes: Avoid cold exposure, stimulants, and smoking. Medications: CCBs (Nifedipine, Amlodipine), ACE inhibitors. Avoid vasoconstrictors (beta-blockers, decongestants, ergotamines). | Complications: Small fingertip/toe ulcers, usually occurs between ages 15-45. |
| Condition | Causes | Signs & Symptoms | Diagnostics | Treatments | Concerns |
|---|---|---|---|---|---|
| Mitral Valve Prolapse (MVP) | Structural valve abnormality, systolic murmur | Fatigue, palpitations, chest pain, lightheadedness (worsens with exertion). May be asymptomatic. Linked to pectus excavatum, joint hypermobility, and Marfan’s syndrome (arm span > height) | Auscultation: Mid-to-late systolic click and murmur Imaging: Echocardiogram with Doppler | Asymptomatic: No treatment needed Symptomatic: Beta-blockers for palpitations, avoid caffeine, alcohol, and smoking Holter monitor: For arrhythmia detection | Complications: Increased risk of thromboembolism, TIA, atrial fibrillation, and ruptured chordae tendineae |
| Hyperlipidemia (HLD) | Risk factors: Hypertension, premature heart disease (women <65, men <55), diabetes, smoking, obesity, microalbuminuria, CAD, PAD | Lipid Levels: – Total cholesterol: Normal <200, Borderline 200-239, High >240 – HDL: >40 (Low HDL often due to high-carb, low-fat diet) – LDL: <100 – Triglycerides: <150 (Risk of pancreatitis if >1000) – If triglycerides >500: Treat first with fenofibrate, niacin, or omega-3s. May be due to metabolic syndrome, diabetes, alcohol abuse, hyperthyroidism, kidney disease, or medications | Screening: – Start fasting lipid tests at 20, repeat every 5 years – If >40, screen every 2-3 years – If diagnosed, screen annually | Lifestyle changes: Exercise, weight loss, healthy fats, no trans fats, reduce junk food, DASH diet, smoking cessation Medications: Focus on lowering LDL unless triglycerides >500 (use statins) Statin interactions: Avoid grapefruit, fibrates, antifungals, macrolides, amiodarone | Risks: Monitor for muscle pain (myalgias), possible memory loss or confusion Elderly: Consider stopping statins at 80+ if symptomatic, though they help prevent MI/CVA by stabilizing atherosclerosis |
| Rhabdomyolysis | Acute skeletal muscle breakdown leading to renal failure | Classic triad: Muscle pain, weakness, and dark urine. Persistent muscle aches without exertion | Tests: – Creatine kinase (CK) – Urinalysis (myoglobinuria, proteinuria) – BUN, creatinine, potassium – EKG (if electrolyte abnormalities suspected) | Management: IV fluids, electrolyte correction, treat underlying cause | Risk factors: Obesity, metabolic disorders, certain medications |
| Nonalcoholic Fatty Liver Disease (NAFLD) | Accumulation of triglycerides in liver | Often asymptomatic, but possible hepatomegaly. If symptomatic: Fatigue, malaise, RUQ pain. Associated with obesity, metabolic syndrome, diabetes, hyperlipidemia | Lab findings: Elevated ALT/AST, negative viral hepatitis (A, B, C) Gold standard: Liver biopsy | Treatment: Weight loss, diet modification, alcohol cessation, avoid hepatotoxic drugs (acetaminophen, statins). Refer to GI for further evaluation | Concerns: Can progress to cirrhosis Most common liver disease in the U.S. Leading cause of liver transplants |
| Varicose Veins | Inherited venous valve defects, prolonged standing, leg crossing, tight clothing, heavy lifting | Enlarged, tortuous superficial veins. Leg aching and mild swelling (worse at the end of the day and in warm weather). Great saphenous vein is most commonly affected | Clinical exam | Treatment options: Laser ablation, sclerotherapy, surgery | Risk factors: Women affected twice as often as men |
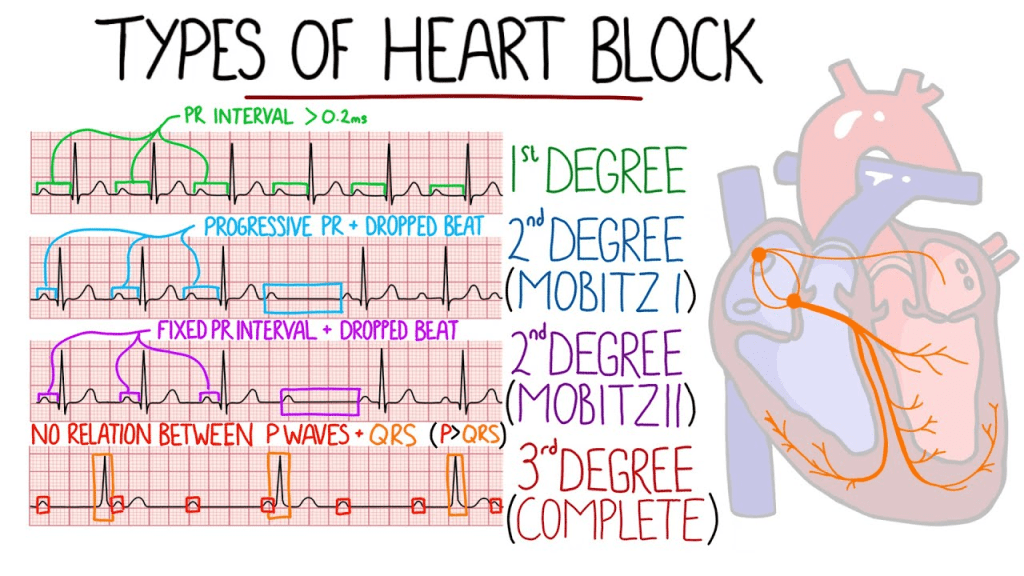
Heart Block
- First-Degree AV Block: The PR interval is prolonged (>0.2 seconds) but remains consistent without dropped beats.
- Mnemonic: “If the R is far from P, then you have First Degree.”
- Second-Degree Type I (Wenckebach): The PR interval gradually lengthens until a QRS complex is dropped.
- Mnemonic: “Longer, longer, longer, drop—then you have Wenckebach.”
- Second-Degree Type II (Mobitz II): The PR interval remains constant, but some QRS complexes are intermittently dropped.
- Mnemonic: “If a QRS doesn’t get through, then you have Mobitz II.”
- Third-Degree (Complete Heart Block): No correlation between P waves and QRS complexes; atria and ventricles beat independently.
- Mnemonic: “If Ps and Qs don’t agree, then you have Third Degree.”