Pneumonia – CURB-65 Assessment
- Confusion: Sudden onset
- Blood Urea Nitrogen: Greater than 19 mg/dL
- Respiratory Rate: Exceeds 30 breaths per minute
- Blood Pressure: Diastolic below 90 mmHg or systolic under 60 mmHg
- Age: 65 years or older
CURB-65 Scoring & Management
- 0-1 points: Outpatient treatment recommended
- 2 points: Consider brief hospitalization or close outpatient monitoring
- 3-5 points: Hospital admission necessary; assess ICU need
ASTHMA/COPD
| Condition | Medication Type | Examples | Usage Guidelines |
|---|---|---|---|
| COPD | LAMA (Long-Acting Muscarinic Antagonist) | -ium (e.g., tiotropium), glycopyrrolate | First-line bronchodilator for stable COPD; used daily for maintenance |
| LABA (Long-Acting Beta-2 Agonist) | -terol (e.g., salmeterol, formoterol) | Often combined with LAMA for moderate to severe COPD | |
| LABA/LAMA Combo | e.g., umeclidinium/vilanterol | Preferred initial therapy in symptomatic patients; improves lung function and reduces exacerbations | |
| ICS (Inhaled Corticosteroids) | -one, -ide (e.g., fluticasone, budesonide) | Reserved for patients with high eosinophil count or frequent exacerbations despite dual therapy | |
| Additional Care | Consider annual low-dose CT scan (LDCT) for lung cancer screening in eligible smokers (age 50–80 with 20+ pack-years, quit <15 years ago) | ||
| Asthma | SABA (Short-Acting Beta-2 Agonist) | Rescue inhaler | Use 1-2 times per week; if needed more often, adjust treatment |
Inhaled Muscarinic Antagonists
- Emerging Use: Asthma management
- Well-Established Role: COPD (provides prolonged effect)
- Preventative, Not for Acute Relief: Requires scheduled use
- Short-Acting (SAMA): Ipratropium bromide (Atrovent) – induces bronchodilation
- Long-Acting (LAMA): Tiotropium bromide (Spiriva), Umeclidinium (Ellipta)
- Anticholinergic Side Effects: May exacerbate benign prostatic hyperplasia (BPH)
- If symptoms worsen, switch from LAMA to LABA (e.g., Salmeterol)
Leukotriene Modifiers
- Added Benefit: Helps manage allergic rhinitis, usually alongside inhaled corticosteroids (ICS)
- Requires Daily Consistency: Essential for best results
- Example: Montelukast (Singulair)
Key Physical Exam Findings
Normal Lung Sounds
- Percussion: Resonant
- Breath Sounds:
- Lower lobes – vesicular
- Upper lobes – bronchial
Signs of Consolidation
- Percussion: Dull
- Increased Tactile Fremitus: Ask patient to say “99”
- Breath Sounds: Bronchial or tubular; often late inspiratory crackles that don’t clear with coughing
- Egophony: “Eee” sounds like “ah”
Pleural Inflammation
- Pain: Sharp, localized; worsens with deep breaths, movement, or coughing
- Pleural Friction Rub: Audible, resembles stepping on fresh snow, heard during both inhalation and exhalation
Air Trapping
- Percussion: Hyperresonant
- Tactile Fremitus: Decreased
- Wheezing: Initially expiratory, later inspiratory as well
- Diaphragm Position: Lowered
- Chest Shape: Increased anteroposterior (AP) diameter
Inhaled Corticosteroids (ICS)
- First-Line Therapy: Best choice for controlling persistent asthma
- Daily Use Required: Consistency is key for maximum benefit
| Medication | Low Dose | Medium Dose | High Dose |
|---|---|---|---|
| Beclomethasone (QVAR) | 80–240 mcg | >240–480 mcg | >480 mcg |
| Budesonide (Pulmicort) | 180–540 mcg | >540–1080 mcg | >1080 mcg |
| Fluticasone (Flovent) | 88–264 mcg | 264–440 mcg | >440 mcg |
| Mometasone (Asmanex) | 100–300 mcg | 300–500 mcg | >500 mcg |
Inhaled Corticosteroids & Long-Acting Beta₂ Agonists (ICS/LABA)
- First-line maintenance therapy for moderate to severe persistent asthma
- Black Box Warning: Increased risk of asthma-related death with LABA use
- Daily, consistent use required for maximum effectiveness
- Combination Medications:
- Budesonide + Formoterol (Symbicort)
- Fluticasone + Salmeterol (Advair)
- Mometasone + Formoterol (Dulera)
- Combination Medications:
Clinical Insights
- Pneumonia & Cardiac Strain: Can increase right-sided heart workload, potentially precipitating heart failure in older adults
Asthma Classification
Intermittent Asthma (FEV₁ > 80% predicted)
- Symptoms occur ≤ 2 days per week
Mild Persistent Asthma (FEV₁ > 80% predicted)
- Symptoms occur more than 2 days per week but not daily
- Nighttime symptoms 3-4 times per month
- Minor activity limitations
Moderate Persistent Asthma (FEV₁ 60-80% predicted) – Most Common Type
- Symptoms daily
- Nighttime symptoms at least once per week
- Some activity limitations
Severe Persistent Asthma (FEV₁ < 60% predicted)
- Symptoms throughout the day
- Nighttime symptoms almost every night
- Severe activity limitations
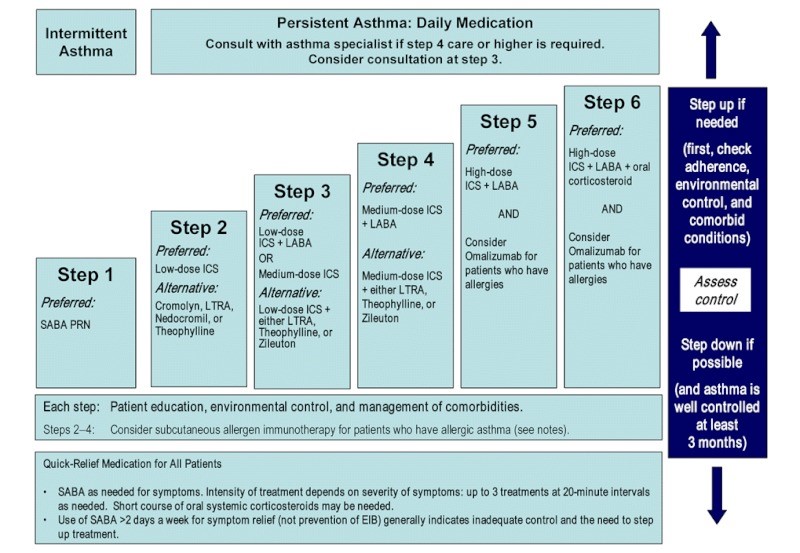
Stepwise Approach to Asthma Management
Asthma treatment has evolved to reduce reliance on short-acting beta₂ agonists (SABAs) alone, even in mild intermittent cases. Current guidelines, including GINA 2023, emphasize the importance of inhaled corticosteroids (ICS) at all stages to reduce the risk of severe exacerbations.
Step 1 (Mild Intermittent Asthma):
- Preferred: As-needed low-dose ICS-formoterol
- Alternative (if ICS-formoterol not available): SABA as needed with concurrent low-dose ICS taken at the same time
Step 2 (Mild Persistent Asthma):
- Daily low-dose ICS
- Alternative: Low-dose ICS-formoterol as needed
- SABA as needed for symptom relief if not using ICS-formoterol
Step 3 (Moderate Persistent Asthma):
- Low-dose ICS + LABA (preferred)
- OR medium-dose ICS
- Consider ICS-formoterol as both maintenance and reliever therapy (SMART approach)
Step 4 (Severe Persistent Asthma):
- Medium-dose ICS + LABA
- Consider add-on therapy such as omalizumab for patients with allergic asthma or other biologics based on phenotype
Step 5:
- High-dose ICS + LABA
- Add oral corticosteroids if needed (lowest effective dose)
- Consider referral for specialist evaluation and biologic therapy (e.g., omalizumab, mepolizumab, dupilumab)
Phosphodiesterase-4 (PDE-4) Inhibitor
- Roflumilast – May cause psychotic symptoms
- Reduces COPD exacerbation risk
COPD: FEV1/FVC < 70
- Significantly increases the workload on the right side of the heart.
| GOLD Stage | Severity | FEV1 (% Predicted) |
|---|---|---|
| GOLD 1 | Mild | >80% |
| GOLD 2 | Moderate | 50% – 80% |
| GOLD 3 | Severe | 30% – 50% |
| GOLD 4 | Very Severe | <30% |
First-Line Therapy:
- GOLD 1-2: (Not commonly seen in the clinic)
- Fewer than one exacerbation per year.
- Low risk: SAMA or SABA as needed.
- High risk: LAMA or LABA on a scheduled regimen.
- GOLD 3-4:
- More than two exacerbations per year.
- ICS + LABA or LAMA on a scheduled regimen.
- Common combination: LAMA + ICS with LABA.
- Long-term oxygen therapy is effective when used for at least 15 hours per day.
Medication Considerations:
- Beta Agonists (SABA: 4 hrs., LABA: 12 hrs.) – Can cause palpitations and tachycardia. Use with caution in patients with hypertension, angina, or hyperthyroidism. Avoid combining with caffeinated beverages.
- Anticholinergics – Prevent bronchoconstriction (-tropium drugs). Avoid in patients with narrow-angle glaucoma, BPH, or bladder neck obstruction.
- Exacerbations – Treated with corticosteroids, with additional medications as needed.
Asthma
Risk Factors for Severe Outcomes
- History of emergency department visits
- Frequent reliance on rescue inhaler
- Nighttime symptoms disrupting sleep
- Progressive worsening of dyspnea and wheezing
- Presence of a respiratory viral infection
Pneumonia Treatment Considerations
- Young, otherwise healthy individuals → Likely atypical pathogens
- First-line: Macrolide or Doxycycline
- Complicated cases → Broader coverage required
- Fluoroquinolone
- OR Macrolide + Beta-lactam
Theophylline
- Acts as a bronchodilator
- Requires consistent daily dosing
Spirometry Interpretation
Obstructive Dysfunction (↓ airflow rates)
- Conditions: Asthma, COPD, Bronchiectasis
Restrictive Dysfunction (↓ lung volume due to reduced lung compliance)
- Causes: Pulmonary Fibrosis, Pleural Disease, Diaphragm Dysfunction
Not recommended during acute exacerbations
Peak Expiratory Flow (PEF)
- Determined by Height, Age, and Gender (HAG)
Cough Evaluation
Duration Matters
- Acute (< 3 weeks):
- Common causes: Respiratory Infection, COPD/Asthma Exacerbation, Pneumonia, Pulmonary Embolism (PE)
- Chronic (> 8 weeks):
- Potential causes: Asthma, GERD, Pertussis, Atypical Pneumonia, Chronic Bronchitis, Bronchiectasis, Lung Cancer
- ACE Inhibitor-induced Cough → Typically begins 1-2 weeks after starting medication
Pulmonary Embolism (PE)
- Most common clinical sign → Tachypnea (rapid breathing)
Chest X-Ray Interpretation
- X-ray Projection:
- PA (Posteroanterior) → X-ray passes from back to front
- AP (Anteroposterior) → X-ray passes from front to back
- Densities on X-ray:
- Air → Appears black (low absorption)
- Bones → Appear white
- Metals → Appear bright white (high absorption)
- Soft tissues → Various gray shades (medium absorption)
- Fluid → Ranges from gray to white
- Structures Visible:
- Trachea, Bronchi, Aorta, Heart, Lungs, Pulmonary Arteries, Diaphragm, Gastric Bubbles, Ribs
Unilateral lung abnormalities warrant imaging
Enlarged hilar nodes require further evaluation
- Trachea, Bronchi, Aorta, Heart, Lungs, Pulmonary Arteries, Diaphragm, Gastric Bubbles, Ribs
Long-Term Steroid Use Risks
- Osteoporosis → Postmenopausal women should take Calcium + Vitamin D (1200 mg daily)
- Growth suppression in children
- Increased risk of eye disorders → Glaucoma, Cataracts
- Immune system suppression
- Adrenal insufficiency due to hypothalamic-pituitary-adrenal (HPA) axis suppression
Stepwise approach to managing asthma
| Condition | Cause | Signs & Symptoms | Diagnostics | Treatment | Key Considerations |
|---|---|---|---|---|---|
| Pulmonary Embolism | History of atrial fibrillation, estrogen therapy, smoking, recent surgery, cancer, pregnancy, long bone fractures, prolonged immobility | Sudden shortness of breath, cough (may produce pink, frothy sputum), tachycardia, pallor, sense of impending doom | Clinical assessment, D-dimer test, CT pulmonary angiography | Anticoagulation therapy, thrombolytics in severe cases, oxygen therapy | Can be life-threatening; requires immediate intervention |
| Impending Respiratory Failure – Asthma Exacerbation | Severe asthma attack leading to respiratory distress | Rapid breathing (tachypnea), abnormal heart rate (tachycardia or bradycardia), cyanosis, anxiety, exhaustion, excessive sweating (diaphoresis), use of accessory muscles for breathing | Cyanosis, diminished lung sounds, difficulty speaking (1-2 words at a time) | Immediate epinephrine, oxygen, nebulized albuterol, IV steroids, antihistamines, H2 blockers | Requires emergency medical attention |
| Chronic Obstructive Pulmonary Disease (COPD) | Alveolar damage due to lung elasticity loss, chronic exposure to irritants, airflow limitation | Persistent cough (2+ years), excessive sputum production, worsening shortness of breath with exertion, barrel chest, weight loss, hyperresonance on percussion, diminished tactile fremitus, reduced egophony, possible coarse crackles | Spirometry (FEV1/FVC < 0.70 post-bronchodilation), alpha-1 antitrypsin screening (if under 45 or significant smoking history), CXR to rule out pneumonia | Smoking cessation, flu/pneumonia vaccines, SABA/LABA/ICS, prednisone (40mg/day for 5-10 days for exacerbations), antibiotics if signs of infection | High-risk patients: >2 exacerbations/year, FEV1 <50%, hospitalization for COPD in past year |
| Community-Acquired Pneumonia (CAP) | Common pathogens: Streptococcus pneumoniae, Haemophilus influenzae, Mycoplasma pneumoniae, Chlamydophila pneumoniae; Pseudomonas aeruginosa in cystic fibrosis patients | Sudden high fever, chills, productive cough (rust-colored sputum if S. pneumoniae), pleuritic chest pain, dyspnea, abnormal breath sounds (rhonchi, crackles, wheezing), dullness over affected lung, increased tactile fremitus, egophony, abnormal whispered pectoriloquy | Chest X-ray (lobar consolidation), CBC (leukocytosis >10.5, check for anemia) | S. pneumoniae: Macrolides, doxycycline; DRSP: High-dose amoxicillin or respiratory fluoroquinolones; Minimum 5-day course | Flu vaccine (>50 y/o), pneumococcal vaccine (>65 y/o), consider lung cancer if recurrent pneumonia |
| Atypical Pneumonia | Mycoplasma pneumoniae, Chlamydophila pneumoniae, Legionella | Gradual onset, fatigue, persistent dry cough, mild symptoms resembling a cold, patients often remain active despite illness, wheezing, diffuse crackles, rhinorrhea, erythematous throat | Physical exam, chest X-ray (diffuse infiltrates), CBC | Macrolides, respiratory fluoroquinolones, doxycycline; supportive care with antitussives, fluids, and rest | Legionella infection linked to contaminated water sources; may present with GI symptoms |
| Acute Bronchitis | Viral infection causing inflammation of the upper respiratory tract | Sudden onset of dry cough (may produce small amounts of sputum), frequent coughing fits, possible low-grade fever, wheezing, chest pain with coughing, cough disrupting sleep | Clinical history, chest X-ray if needed | Symptomatic relief: Dextromethorphan, Tessalon Perles, guaifenesin; severe wheezing may require Atrovent or albuterol inhaler; consider short-course steroids (40mg for 3-5 days) | May exacerbate asthma; secondary bacterial infections can lead to pneumonia; rarely requires antibiotics (macrolide or doxycycline only in select cases) |
| Pertussis (Whooping Cough) | Bordetella pertussis bacterial infection | Persistent cough lasting >14 days with at least one of the following: severe coughing fits (paroxysms), inspiratory whooping sound, vomiting after coughing; progresses through three stages (catarrhal, paroxysmal, convalescent); most contagious in early stages | Nasal swab (PCR, culture), pertussis antibodies (ELISA), CBC (lymphocytosis >80%) | Macrolides (first-line treatment), prophylactic treatment for close contacts, respiratory precautions, symptomatic relief (antitussives, mucolytics, rest, hydration) | Tdap booster recommended (>11 years old); complications include sinusitis, otitis media, pneumonia, fainting, rib fractures |
| Tuberculosis | Mycobacterium tuberculosis | Fever, loss of appetite, fatigue, night sweats, persistent cough. Progresses to productive cough with blood-streaked sputum and unexplained weight loss. | Mantoux test: Positive if induration >10mm QuantiFERON or T-SPOT IGRA: Available within 24 hours Sputum: Collect for 3 days – NAAT, C&S, AFB CXR: Upper lobe involvement | Report to health department Treatment based on Mantoux test results: >5mm: High-risk individuals (HIV+, recent contact, immunocompromised) >10mm: Immigrants, young children, IV drug users, healthcare workers, homeless, inmates >15mm: Low-risk individuals Medications: Isoniazid (INH) 300mg daily, rifampin, ethambutol, pyrazinamide (3x weekly) Monitor liver function. | Risk Factors: HIV, migrants, homeless populations, inmates, nursing home residents BCG vaccine history: May cause false positive Ethambutol caution: Can cause optic neuritis; avoid in patients with visual impairment. |
| Asthma | Chronic inflammation of bronchial tree Reversible condition. | Recurrent cough, wheezing (especially at end of exhalation), breathlessness, and chest tightness due to variable airflow obstruction and bronchial hyperresponsiveness. Symptoms worsen at night, with exercise, viral infections, or smoke exposure. Often begins in childhood. Asthma triad: Wheezing, coughing, and shortness of breath. | Spirometry: FEV1 increase >12% after bronchodilator Pulmonary function test (PFT): Assesses treatment response and severity | Rescue medications: Short-acting beta agonists (SABA) Long-term control: Inhaled corticosteroids Step-up therapy if symptoms are uncontrolled Acute exacerbation: Prednisone 40-60mg/day for 3-10 days Peak flow monitoring to track control Follow-ups: Every 3-6 months if well controlled; every 2-6 weeks if not controlled Annual check-ups recommended in September to adjust medication and update immunizations. | Bone health: Consider bone density monitoring for long-term steroid use Goals of treatment: – Maintain normal activity levels – Minimize exacerbations – Limit rescue inhaler use (<2 days per week) – Avoid emergency room visits – Maintain normal pulmonary function test (PFT) results. |
Lung Cancer Screening Guidelines
Common Symptoms
- Persistent chest pain or discomfort
- Shortness of breath (dyspnea)
- Coughing up blood (hemoptysis)
- Chronic cough
High-Risk Individuals
- Ages 55-74 with a history of at least 30 pack-years of smoking, including those who quit within the past 15 years
- Smokers aged 50+ considered at higher risk
Current Challenges & Limitations
- Frequent false positives, leading to unnecessary testing
- Cumulative radiation exposure from repeated CT scans
- Increased patient anxiety due to screening uncertainties
| Asthma | COPD | |
| X | Consider steroid first for treatment | |
| X | Anticholinergics are not usually helpful | |
| Disease is progressive | X | |
| Never | LABA alone is safe | X |
| X | Steroid alone is safe | |
| X | Needs rescue inhaler | X |