Constipation
Common Causes
• Functional or idiopathic origins
• Lifestyle factors:
- Sedentary behavior
- Low-fiber diet
- Inadequate hydration
- Excessive dairy consumption
- Ignoring the urge to defecate
Medications That May Contribute
• Iron supplements
• Beta-blockers
• Calcium channel blockers
• Antihistamines
• Anticholinergics
• Antipsychotics
• Opioids
• Calcium-based antacids
Management Strategies
• Establish a regular bowel routine
• Adopt a fiber-rich diet (25-35 g/day)
• Stay physically active
• Maintain proper hydration (8-10 glasses of water daily)
• Use laxatives if necessary
Anal Fissure
Description
• A small tear or ulcer in the anal canal, typically located posteriorly
Symptoms
• Intense, sharp pain during bowel movements (often described as feeling like razor blades)
• Pain that persists for hours after defecation, leading to constipation due to fear of pain
• Small amounts of blood on toilet paper after wiping
Risk Factors
• Chronic constipation or straining
• Frequent diarrhea
• Childbirth
• Anal intercourse
Treatment Approach
• Prevent constipation:
- Increase dietary fiber intake
- Use laxatives if needed (e.g., mineral oil, but avoid long-term use due to interference with vitamin A, D, E, and K absorption)
• Sitz baths and cool compresses for symptom relief
• If conservative measures fail, consider topical nitroglycerin (NTG), Botox injections, or surgical sphincterotomy
Hemorrhoids
Classification:
- Grade I: No prolapse
- Grade II: Prolapse during bowel movements but retracts on its own
- Grade III: Prolapse with defecation, requiring manual reduction
- Grade IV: Permanently prolapsed and cannot be manually repositioned
Risk Factors:
- Heavy alcohol consumption
- Persistent constipation or diarrhea
- Obesity
- Diet high in fat and low in fiber
- Prolonged sitting or sedentary habits
- Anal intercourse
- Weakening of pelvic floor muscles
Hepatitis Serology Overview
Antibody Basics:
- IgG (“Gone”) – Appears after infection clears; indicates past exposure and immunity. No active virus.
- IgM (“Minute”) – First antibody produced during infection; signals an active, contagious stage with no established immunity.
Hepatitis A (HAV):
- Spread via ingestion of contaminated food or water.
- Anti-HAV IgG positive → Immunity to HAV (past infection or vaccination).
- Anti-HAV IgM positive → Active infection.
- Both IgM & IgG negative → No immunity; vaccination recommended.
Hepatitis B (HBV):
- HBsAg (Surface Antigen): Indicates the presence of the Hep B virus (active infection).
- Anti-HBs (Surface Antibody): Confirms immunity (recovery or vaccination).
- Anti-HBc (Core Antibody): Suggests past or present infection (“rotten to the core”).
- IgM Anti-HBc: Suggests recent or ongoing infection.
Hepatitis C (HCV):
- Primarily linked to injection drug use.
- Anti-HCV Test: Initial screening for Hep C exposure.
- If negative → No infection.
- If positive → Confirm with HCV RNA or PCR to check for chronic infection.
- If HCV RNA/PCR positive → Chronic Hep C → Referral recommended.
- Routine screening advised for individuals born between 1945-1965.
Hepatitis D (HDV):
- Only occurs in those already infected with Hep B.
- Can be acute or chronic.
- Coinfection with Hep B & D increases the likelihood of cirrhosis and liver damage.
Abdominal Maneuvers Indicating Appendicitis
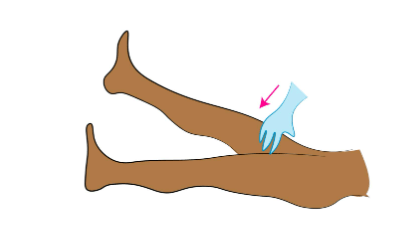
Psoas (Iliopsoas) Sign:
- Patient lies supine with hip flexed at 90°.
- Pain occurs when the patient pushes against resistance or when the leg is extended.
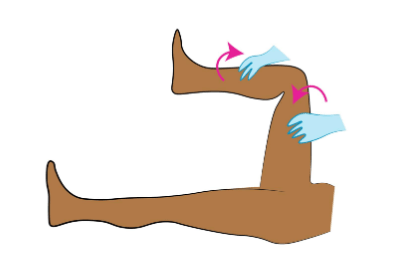
Obturator Sign:
- Patient in a supine position.
- Internally rotate the right hip through its full range of motion.
- Pain with movement or hip flexion suggests appendicitis.
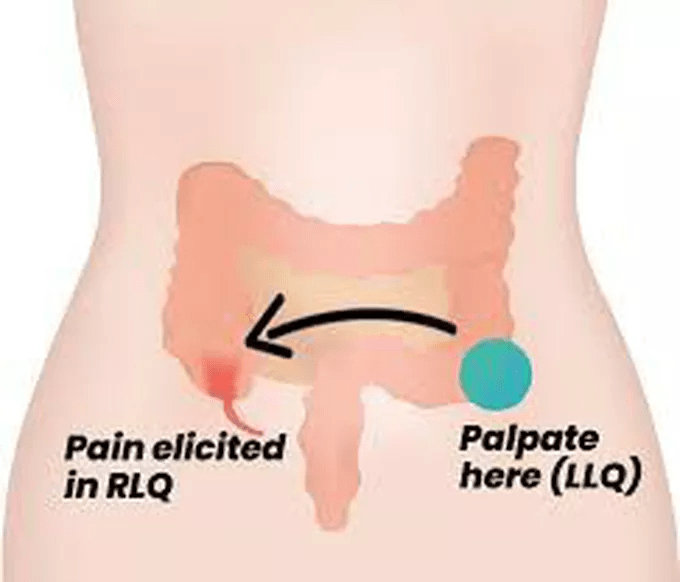
Rovsing’s Sign:
- Deep palpation of the left lower quadrant (LLQ) causes referred pain in the right lower quadrant (RLQ).
McBurney’s Point Tenderness:
- Located in the RLQ, midway between the superior iliac crest and the umbilicus.
- Tenderness in this area is a classic sign of appendicitis.

Abdominal Assessment Maneuvers
Markle Test (Heel Jar Sign):
- Patient stands on tiptoes and then drops suddenly onto heels or jumps.
- Test is positive if pain is triggered or the patient refuses due to discomfort.
Involuntary Guarding:
- Reflexive tightening of abdominal muscles upon palpation.
Rebound Tenderness (Blumberg’s Sign):
- Increased pain occurs when the examining hand is suddenly released after deep palpation.
Murphy’s Sign:
- Press deeply into the right upper quadrant (RUQ) beneath the costal margin during inspiration.
- A positive sign is mid-inspiratory arrest due to pain.
Cullen’s Sign:
- Bluish discoloration and swelling around the umbilicus, suggestive of internal bleeding.
Grey Turner’s Sign:
- Bluish discoloration of the flanks, potentially indicating retroperitoneal hemorrhage.
Liver Function Tests (LFTs)
Aspartate Aminotransferase (AST) / Serum Glutamic-Oxaloacetic Transaminase (SGOT):
- Found in liver, heart, muscles, kidneys, and lungs.
Alanine Aminotransferase (ALT) / Serum Glutamic-Pyruvic Transaminase (SGPT):
- Primarily located in the liver.
- Elevated ALT suggests liver inflammation—more specific for hepatic issues.
AST vs. ALT Elevation Patterns:
- ALT > AST → Think hepatitis (liver-related).
- AST > ALT → Consider acetaminophen toxicity, statin use, or excessive alcohol intake (tequila).
AST/ALT Ratio:
- ≥2.0 → Suggests alcohol-related liver damage.
- 1–2 → May indicate alcohol-related or other liver disease.
- <1 → Often associated with fatty liver disease.
Serum Gamma-Glutamyl Transferase (GGT):
- Increased in chronic alcohol use and acute pancreatitis.
- Highly sensitive marker for alcohol abuse.
Alkaline Phosphatase (ALP):
- Enzyme found in bones, liver, gallbladder, kidneys, gastrointestinal tract, and placenta.
- Elevations occur with growth spurts, bone healing, osteomalacia, vitamin D deficiency, Paget’s disease, and bone cancer.
- Naturally higher in pregnancy and children.
Albumin:
- Produced by the liver—a key marker of hepatic function.
| Name | Cause | Signs/Symptoms | Diagnostics | Treatments | Concerns |
|---|---|---|---|---|---|
| Acute Appendicitis | Inflammation due to infection or obstruction | Sudden periumbilical pain that worsens over 12-24 hours, shifting to McBurney’s point with rebound tenderness and guarding. Positive Psoas and obturator signs. If ruptured, presents with a rigid abdomen, severe guarding, and rebound tenderness. | CT with contrast; Ultrasound (preferred for younger, thinner patients); Bloodwork: Elevated WBC, neutrophils, and bands. | Immediate surgical referral. | Common in ages 10-30. Presence of immature neutrophils (myelocytes/metamyelocytes) may indicate life-threatening infection in rupture cases. |
| Acute Cholecystitis | Inflammation of the gallbladder, usually from gallstones | Persistent severe RUQ or epigastric pain, which can be colicky and worsen within an hour of eating fatty foods. Pain may radiate to the right shoulder, accompanied by nausea, vomiting, anorexia, intermittent fever, and positive Murphy’s sign. | Elevated AST, ALT, ALP; RUQ ultrasound; HIDA scan. | Rest gut with clear liquids; surgical referral. | Higher risk in individuals who are fair-skinned, overweight, and over 40. Cholelithiasis (stones without inflammation) can also occur. |
| Acute Diverticulitis | Infection of diverticula in the colon (most common in the sigmoid) | Fever, nausea, anorexia, cramping, and LLQ pain. Positive Blumberg’s and Rovsing’s signs, with a board-like abdomen in severe cases. Diverticulosis itself is often asymptomatic. By age 50, around 33% of people develop diverticulosis. | CBC: Leukocytosis with neutrophilia; FOBT positive if bleeding; CT scan (definitive). | Ciprofloxacin + Metronidazole (10-14 days) or Levaquin + Flagyl. High-fiber diet, follow-up in 48-72 hours. Severe cases require ER referral. | Risk factors: Aging, low fiber intake, obesity, sedentary lifestyle, NSAID use, family history, connective tissue disorders. Complications: Sepsis, bowel obstruction, perforation, fistula, hemorrhage, death. |
| Acute Pancreatitis | Causes include excessive alcohol consumption, gallstones, drug use, hypertriglyceridemia, or infections. | Sudden onset of severe upper abdominal pain radiating to the mid-back, bloating, nausea, vomiting, and fever. Guarding and epigastric tenderness are common. Cullen’s sign and Grey-Turner’s sign may be present. Patients may rock back and forth to relieve pain. | Elevated serum amylase, lipase, and trypsin; AST, ALT, GGT, bilirubin, and WBCs also elevated; Abdominal ultrasound and CT; Triglycerides >800 increase risk. | Immediate referral. | Can progress to ileus, sepsis, shock, multi-organ failure. Chronic pancreatitis, smoking, and diabetes increase the risk of pancreatic cancer. |
| Clostridium difficile Colitis (C-diff) | Infection, often following antibiotic use (clindamycin, quinolones, cephalosporins, penicillins). | Severe watery diarrhea (10-15 stools/day), lower abdominal pain, cramping, and fever. Symptoms develop 5-10 days after starting antibiotics. | CBC: Leukocytosis (>15,000); Stool assay for C. difficile toxin. | Metronidazole (Flagyl), increased fluid intake; avoid antimotility agents and opioids. | Can lead to severe dehydration, toxic megacolon, or colonic perforation if untreated. |
| Colon Cancer | Adenocarcinoma, the third leading cause of cancer deaths in the U.S. | Often asymptomatic until advanced stages. May present with changes in bowel habits, GI discomfort, blood in stool (heme-positive or dark/tarry stools), and palpable abdominal mass. History of polyps increases risk. | Colonoscopy at age 50 (repeat every 10 years unless polyps are present); Under 40, assess cancer risk; FOBT annually; Cologuard every 3 years. | Screening questions: History of colorectal cancer (CRC) or adenomatous polyps? Inflammatory bowel disease? Family history of CRC/AP? Treatment includes surgery, chemotherapy, and radiation. | Risk factors: Age >50, multiple polyps, inflammatory bowel disease, diets high in fat and red meat, low calcium intake. |
| Crohn’s Disease | Chronic inflammatory bowel disease affecting any part of the digestive tract, from mouth to anus. Inflammation affects the entire intestinal wall. | Symptoms include fever, fatigue, mild weight loss, RLQ pain, and a tender abdominal mass. Remissions and relapses are common. If the ileum is involved, diarrhea is non-bloody. If the colon is affected, bloody diarrhea with mucus occurs. May cause fistula formation and anal disease. | Increased CRP, ESR, and WBCs; Anemia (due to chronic disease or B12 deficiency); WBCs in stool; Endoscopy shows cobblestone mucosa and ulcers. | Lactulose intolerance is common; smoking cessation is essential. Gut rest, oral aminosalicylates (sulfasalazine, mesalamine), Flagyl, Cipro, and immune modulators. | Risk of toxic megacolon and colon cancer. Higher lymphoma risk when treated with azathioprine. More common in Jewish populations. |
| Ulcerative Colitis | Chronic inflammation limited to the colon and rectum, affecting only the mucosa. | Symptoms include bloody diarrhea with mucus, severe cramping (especially on the left side), bloating, and gas, worsened by food intake. Relapses may cause fever, anorexia, weight loss, and fatigue. Associated with arthritis in large joints and ankylosing spondylitis. May result in iron-deficiency anemia (IDA) or anemia of chronic disease. | Increased CRP, ESR, and WBCs; Anemia; WBCs in stool. | Oral aminosalicylates (sulfasalazine, mesalamine), corticosteroids. Antibiotics are avoided due to C. difficile risk. Immune modulators may be required. | Increased risk of toxic megacolon and colon cancer. |
| Name | Cause | Signs/Symptoms | Diagnostics | Treatments | Concerns |
|---|---|---|---|---|---|
| Zollinger-Ellison Syndrome | Gastrinoma in the pancreas or stomach leading to excessive gastrin secretion | High stomach acid production, ulcers in the stomach and duodenum, epigastric to mid-abdominal pain, tarry stools | Fasting gastrin levels | ||
| GERD | Weak lower esophageal sphincter (LES), esophageal irritation, increased gastric acid production | Chronic heartburn, worsens after large/fatty meals and when lying down, recurrent dry cough, chronic pharyngitis, hoarseness, OTC antacid/H2 blocker use | Clinical diagnosis; endoscopy if dysphagia, odynophagia, unintended weight loss, hematemesis, melena, chest pain, or choking | Lifestyle modifications (avoid eating before bedtime, dietary changes, weight loss), avoid triggers (mints, chocolate, alcohol, aspirin, NSAIDs, caffeine, carbonated drinks). Medications: antacids, H2 blockers, PPIs | Chronic GERD may lead to Barrett’s esophagus and increased risk of esophageal cancer. Long-term PPI use linked to hip fractures, pneumonia, and C. diff infection. |
| Irritable Bowel Syndrome (IBS) | Functional disorder of the colon (spastic colon) | Intermittent cramping, especially LLQ, bloating, flatulence, relief after defecation, alternating diarrhea and constipation, stress-induced flare-ups | Abdominal tenderness, R/O infections, Rome III criteria | Increase fiber, avoid gas-producing foods, antispasmodics, fiber supplements or Miralax (for constipation), Imodium (for diarrhea), stress management | More common in females |
| Erosive Gastritis (Gastric Ulcer) | H. pylori, stress, alcohol, NSAID overuse | Epigastric pain (burning/gnawing), worse after eating, tenderness at epigastrium, dysphagia, early satiety, weight loss | Endoscopy if concerning symptoms present | H. pylori-negative: Stop NSAIDs, alcohol, smoking, stress management, H2 blockers, PPIs. H. pylori-positive: Triple therapy (Clarithromycin + Amoxicillin + Omeprazole or Flagyl if allergic to Amoxicillin) for 14 days | Sudden medication discontinuation can worsen symptoms |
| Duodenal Ulcer | H. pylori infection | Burning/gnawing epigastric pain, relieved by food or antacids but recurs 2-3 hours later, symptoms worsen at night (1-2 AM) | H. pylori stool antigen test or urea breath test (serology not recommended) | H. pylori transmitted via oral-fecal and oral-oral routes | |
| Viral Hepatitis | A: Fecal-oral; B: Blood, sexual, mother-to-child; C: IV drug use, blood transfusion | Fatigue, nausea, anorexia, malaise, abdominal pain, dark urine, clay-colored stools, jaundice, tender liver | Elevated ALT/AST (up to 10x normal) | Avoid hepatotoxic substances (Tylenol, alcohol, statins), supportive treatment | Reportable disease. Hepatitis A: Prevent with vaccination, post-exposure prophylaxis available. Hepatitis B: Treat with PEG-IFN-a, entecavir, or tenofovir; post-exposure HBIG and vaccination. Hepatitis C: Screen baby boomers (1945-1965), treat with antivirals (Harvoni, ribavirin, pegylated interferon). Chronic Hep C can cause liver cancer and transplant need. |