Elderly
Distinguishing delirium from dementia
| Feature | Delirium | Dementia |
|---|---|---|
| Definition | A sudden and rapid decline in brain function, leading to confusion, changes in cognition, activity levels, and level of consciousness (LOC). | A slow and progressive decline in intellectual or cognitive function that worsens over time and interferes with daily activities. |
| Cause | Typically triggered by an acute underlying condition, such as an infection or illness. | Can result from a variety of causes, often related to neurodegenerative diseases. |
| Onset | Develops quickly over hours to days. | Gradual onset with no specific starting point; symptoms progress over time. |
| Memory | Impaired but inconsistent—recall may vary. | Progressive memory loss, particularly affecting recent events. |
| Duration | Lasts hours to days. | Persists for months to years. |
| Reversibility | Usually reversible if the underlying cause is treated. | Typically progressive and irreversible. |
| Sleep Patterns | Sleep-wake cycle is disrupted, with fluctuations in alertness; symptoms often worsen later in the day (“sundowning”). | Sleep disturbances are present but without sudden fluctuations; may include a day-night reversal. |
| Psychomotor Activity | Changes in movement—may be hyperactive, hypoactive, or a combination of both; 15% of cases show no change. | Typically normal until the later stages of the disease. |
| Perceptual Disturbances | Hallucinations and other sensory misinterpretations are common. | Absent in early stages but may appear as the disease progresses. |
| Speech | Often incoherent, confused, or nonsensical. | Generally unaffected in early stages but deteriorates over time. |
Causes and management of delirium
Potential causes:
- Medications – Delirium can occur when new drugs are introduced or dosages are modified. Common culprits include anticholinergics, tricyclic antidepressants (TCAs), antihistamines, antipsychotics, opioids, benzodiazepines, alcohol, and other central nervous system depressants.
- Emotional factors – Mood disturbances, grief, or significant loss.
- Electrolyte imbalances – Conditions such as hyponatremia.
- Oxygen deprivation – Can result from pneumonia, chronic obstructive pulmonary disease (COPD), myocardial infarction (MI), or pulmonary edema.
- Withdrawal or lack of necessary medications.
- Infections – Urinary tract infections (UTIs) and pneumonia are common triggers.
- Urinary or fecal retention.
- Reduced sensory stimulation – Vision or hearing impairment, darkness, or unfamiliar environments.
- Seizure-related states – Ictal or post-ictal confusion.
- Nutritional deficiencies – Protein-calorie malnutrition, vitamin B12 or folate deficiency, or dehydration.
- Metabolic disorders – Diabetes, thyroid dysfunction, or myocardial infarction (MI).
- Subdural hematoma.
Management:
- Identify individuals most at risk.
- Address and treat the underlying cause.
Causes of dementia
- Alzheimer’s disease – Accounts for 50-80% of cases, primarily affecting executive function.
- Vascular dementia – Represents approximately 20% of cases, often occurring after a stroke and leading to memory impairment.
- Parkinson’s disease-related dementia – Affects around 5% of individuals with dementia.
- Other causes – Includes conditions such as HIV-associated neurocognitive disorders, dialysis-related encephalopathy, neurosyphilis, normal pressure hydrocephalus, Pick’s disease, Lewy body dementia, and frontotemporal dementia.
Cancer in aging populations
- Lung and bronchial cancer is the leading cause of cancer-related death in both sexes. The primary risk factor is smoking, and non-small cell lung carcinoma accounts for about 90% of cases. Patients with a persistent cough should receive a chest X-ray followed by a CT scan. Diagnosis is confirmed with a positive lung biopsy. Initial workup may include CBC, FOBT, chemistry panel, and urinalysis. Referral to a pulmonologist for bronchoscopy and biopsy is indicated. According to the 2021 USPSTF guidelines, annual low-dose CT screening is recommended for adults aged 50–80 with a ≥20 pack-year smoking history who currently smoke or have quit within the past 15 years.
- Second leading cause of cancer-related death: Colorectal cancer – At the time of diagnosis, about 20% of cases already have distant metastases. Risk factors include increasing age, inflammatory bowel disease, family history of colorectal cancer, colonic polyps, sedentary lifestyle, high-fat and low-fiber diet, and obesity. Patients presenting with altered bowel habits should undergo baseline tests such as CBC, FOBT, chemistry panel, and UA, with a referral to a gastroenterologist. Screening recommendations:
- Baseline colonoscopy at age 45 (repeat every 10 years).
- Sigmoidoscopy every 5 years.
- Cologuard every 3 years for low-risk individuals.
- FOBT annually.
Guidelines for Alzheimer’s care
- Slowing cognitive decline:
- Vitamin E 1000U twice daily
- Selegiline 5mg twice daily
- Managing mild to moderate Alzheimer’s disease:
- Cholinesterase inhibitors:
- Donepezil (Aricept)
- Rivastigmine (Exelon)
- Galantamine (Razadyne)
- These medications offer modest benefits.
- Cholinesterase inhibitors:
- For advanced stages:
- N-methyl-D-aspartate (NMDA) receptor antagonist:
- Memantine (Namenda)
- N-methyl-D-aspartate (NMDA) receptor antagonist:
- Addressing agitation and depression
- Investigating non-Alzheimer’s causes of behavioral changes:
- Pain or infections as potential contributors
- When environmental adjustments are ineffective:
- Psychotropic medication (e.g., risperidone) may be considered.
Recognizing and addressing elder abuse
- Physical signs:
- Unexplained bruises, skin tears, lacerations, or fractures.
- Indicators of possible sexual abuse:
- Presence of sexually transmitted infections.
- Vaginal or rectal bleeding.
- Bruising on the breasts.
- Neglect-related signs:
- Malnutrition, inadequate hygiene, and pressure ulcers.
- Assessment considerations:
- Screen for potential abuse and financial exploitation.
- Conduct private interviews with the elder, asking:
- “Do you feel safe in your home?”
- “Who is responsible for managing your finances?”
- “Who prepares your meals?”
Key insights on aging and elderly health
- Top three causes of mortality in individuals over 65:
- Cardiovascular disease – Includes myocardial infarction (MI), heart failure, and arrhythmias.
- Cancer – Most commonly lung and colorectal cancer.
- Chronic lower respiratory diseases – Primarily chronic obstructive pulmonary disease (COPD).
- Demographic trends:
- The fastest-growing age group is 85 and older.
- Individuals aged 65 to 74 are classified as the “young-old.”
- Key clinical considerations:
- Unexplained iron-deficiency anemia in older adults, particularly males or postmenopausal women, warrants a colonoscopy referral to rule out gastrointestinal malignancy.
- Elevated calcium or alkaline phosphatase levels in lab results may indicate bone metastases from cancer.
- Depression is frequently associated with dementia.
- Cholinesterase inhibitors may cause nausea and diarrhea as side effects.
- Common geriatric symptoms:
- Syncope (fainting episodes).
- Dizziness and balance issues.
- Vertigo (a sensation of spinning or motion).
Essential daily living skills
- Basic self-care abilities:
- Independent eating and nutrition management.
- Control over bowel and bladder functions.
- Personal hygiene, including bathing and grooming.
- Advanced daily living skills (Instrumental ADLs):
- Shopping for groceries and essentials.
- Performing household chores and upkeep.
- Handling personal finances and budgeting.
- Communicating via telephone or other devices.
- Operating a vehicle or arranging transportation.
Medications to avoid in older adults
- Drugs with anticholinergic effects:
- Tricyclic antidepressants
- Medications for overactive bladder
- First-generation antihistamines
- Common side effects:
- Dry as a bone – Dry mouth and eyes
- Red as a beet – Skin flushing
- Mad as a hatter – Confusion and cognitive impairment
- Hot as a hare – Increased body temperature
- Can’t see – Vision disturbances
- Can’t pee – Urinary retention
- Can’t spit – Dry mouth
- Can’t shit – Constipation
- Medications with high risks in elderly populations:
- Tricyclic antidepressants – Can cause significant orthostatic hypotension.
- Sedative-hypnotics (sleep aids) – Increased risk of falls and fractures.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) – May exacerbate fluid retention.
- Selective serotonin reuptake inhibitors (SSRIs) – Can contribute to hyponatremia; elderly patients should be monitored after one month, especially if also taking thiazide diuretics.
- Use with caution in patients with:
- Benign prostatic hyperplasia (BPH)
- Narrow-angle glaucoma
- Preexisting cardiovascular disease
Evaluating fall risk
- Timed Up and Go (TUG) test
Physiological and metabolic transformations
- Skin and hair:
- Thinning and reduced elasticity due to diminished subcutaneous fat and collagen.
- Increased fragility with delayed wound healing.
- Xerosis (dry skin): Resulting from decreased sebaceous and sweat gland function, heightening susceptibility to dehydration and heat-related illnesses.
- Reduced vitamin D production.
- Fewer melanocytes, leading to graying hair.
Seborrheic keratoses -Noncancerous, soft, wart-like growths with a “stuck-on” appearance. Primarily located on the back. Vary in color from tan to dark brown or black.

Senile purpura – Vividly colored bruises with distinct, well-defined borders.

Lentigines – Commonly known as “liver spots,” these tan to brown pigmented macules appear on the backs of the hands and forearms.

Stasis dermatitis – Skin inflammation resulting from prolonged edema.

Senile actinic keratosis – Caused by prolonged sun exposure, with the potential to develop into squamous cell carcinoma.

Nails – Growth rate decreases, becoming brittle, thickened, yellowish, and marked with longitudinal ridges.
Mouth – Hyposmia – Reduced ability to detect odors.
Physiological and Metabolic Alterations
.Vision changes – Presbyopia results from reduced lens flexibility, making it harder to focus on nearby objects. Typically emerges in the mid-40s, often requiring reading glasses. Greater light requirements, heightened glare sensitivity, and reduced color vibrancy.
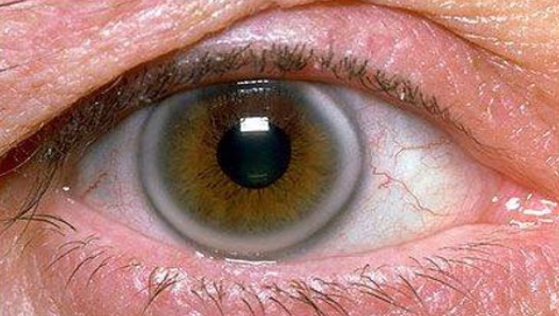
Arcus Senilis – A gradually developing opaque gray or white ring along the corneal margin or iris periphery, unrelated to vision impairment. Caused by cholesterol and fat deposits. If present before age 40, assess fasting lipid levels.
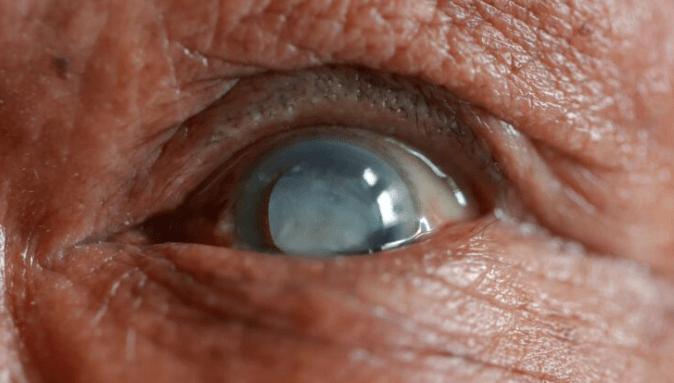
Cataracts – Progressive lens clouding and opacity, leading to impaired vision .Develops gradually, often causing reduced night vision. Red reflex absent upon examination. Leading cause of blindness in developing nations.
Macular degeneration – Progressive deterioration of the macula, resulting in central vision loss. Leading cause of blindness in the United States.
- Ears – Presbycusis (age-related sensorineural hearing loss) primarily affects high-frequency sounds. Onset typically around age 50. Hearing protection recommended in noisy environments to reduce risk.
- Heart – Arteries become elongated and twisted, with thickened intimal layers and arteriosclerosis contributing to increased blood pressure due to higher vascular resistance. Calcium deposits may form on the mitral and aortic valves.
- Baroreceptor sensitivity declines, reducing the body’s ability to adjust to positional changes, increasing orthostatic hypotension risk.
- Maximum heart rate decreases, and the left ventricle hypertrophies over time.
- S4 heart sound may be a normal finding in older adults.
- Lungs – Total lung capacity remains unchanged, but forced vital capacity (FVC) and forced expiratory volume in one second (FEV1) decline with age.
- Residual lung volume increases due to decreased lung and chest wall compliance.
- Chest wall becomes stiffer, and the diaphragm functions less efficiently.
- Mucociliary clearance weakens, reducing the ability to clear secretions.
- Diminished respiratory response to hypoxia and hypercapnia.
- Common to observe decreased breath sounds and basal crackles without underlying disease (often improves with coughing).
- Anteroposterior (AP) diameter increases with aging.
- Liver – Size and mass decrease due to atrophy, with a higher likelihood of fat accumulation.
- Levels of ALT, AST, and alkaline phosphatase remain relatively stable.
- Metabolism of drugs slows, affecting clearance.
- LDL and total cholesterol levels tend to rise with aging.
Physiological and Metabolic Changes with Aging
- Renal System – Kidney size and mass begin declining after age 50. Glomerular filtration rate (GFR) starts decreasing by age 40, with up to 30% of renal function lost by age 70. Drug clearance through the kidneys becomes less efficient. Serum creatinine is an unreliable marker of kidney function due to reduced muscle mass, creatine production, and creatinine clearance. NSAID-induced kidney damage risk is significantly higher, and renin-angiotensin levels are lower in older adults.
- Genitourinary System – Increased residual urine in the bladder. In postmenopausal women, the urethra becomes thinner and shorter, reducing urinary sphincter tightness, increasing urinary incontinence (which is 2-3 times more common in women). Erectile dysfunction affects 40% of men at age 40 and 70% by age 70.
- Musculoskeletal System – Height loss of 1-3 inches can occur due to bone thinning and vertebral compression fractures, which are indicative of osteoporosis. Morning stiffness that improves with movement suggests osteoarthritis (degenerative joint disease). Fat mass increases while muscle mass and strength decline. Bone loss occurs faster in women than men (4:1 ratio). Fractures take longer to heal because osteoblast activity (bone formation) decreases while osteoclast activity (bone breakdown) remains high.
- Gastrointestinal System – Gum recession and dry mouth are common. Taste bud sensitivity declines, reducing appetite. Absorption efficiency for folic acid, vitamin B12, and calcium decreases in the small intestine. Delayed gastric emptying can contribute to indigestion. Lower prostaglandin production increases the risk of gastritis and gastrointestinal damage. Constipation is more frequent due to slower colonic transit time, and fecal incontinence may occur due to medications or medical conditions. Laxative misuse is more prevalent in older adults.
- Endocrine System – Mild pancreatic atrophy occurs with age. Increased insulin levels with mild peripheral insulin resistance are common. Alterations in circadian rhythm hormone secretion contribute to sleep disturbances.
- Sex Hormones – The testes remain functional throughout life, but DHEA and testosterone production decline. In women, estrogen and progesterone levels drop significantly after menopause.
- Immune System – Older adults are less likely to develop a fever during infections. Antibody response to vaccines weakens, and overall immune function declines. Cell-mediated immunity (T-lymphocytes, macrophages, cytokines) is more affected by aging than humoral immunity (B-lymphocytes and antibody production).
- Hematologic System – No significant changes in red blood cell lifespan, blood volume, or circulating lymphocytes. Increased risk of thrombi and emboli due to heightened platelet responsiveness. Iron and folate-deficiency anemia risk rises, as gastrointestinal absorption of vitamin B12 and folate diminishes.
Age-Related Physiological and Metabolic Adaptations
- Neurological System – Changes in color perception, altered pupillary response, and diminished corneal reflex. Reduced gag reflex is common. Deep tendon reflexes may be either exaggerated or absent. Neurological assessments can be influenced by medications, leading to slower reaction times. Benign essential tremors are frequently observed in older adults.
- Pharmacokinetics and Drug Metabolism – Drug clearance declines due to renal insufficiency, reduced liver efficiency, delayed gastric emptying, increased gastric pH, and decreased serum albumin levels. Medications such as warfarin (Coumadin) and phenytoin (Dilantin) require dosage adjustments due to lower albumin levels. Higher fat-to-muscle ratio alters drug distribution. Older adults are more sensitive to benzodiazepines and anticholinergic drugs (including hypnotics, tricyclic antidepressants, antihistamines, and antipsychotics). Absorption rates change, beta-2 receptor sites decline, and sodium conservation ability decreases with age.
Cognitive and Neurological Impairments
- Abulia – Lack of motivation or interest in performing tasks, accompanied by indifference to social expectations.
- Akathisia – Overwhelming urge to move due to extreme restlessness.
- Akinesia – Decrease in voluntary muscle activity.
- Amnesia – Memory loss. Anterograde amnesia affects the ability to recall recent events (occurs with disease progression), whereas retrograde amnesia impacts memories from before disease onset.
- Anomia – Difficulty retrieving words or names.
- Aphasia – Impairment in speech production and/or comprehension, including spoken and written language.
- Apraxia – Loss of ability to perform learned motor tasks.
- Astereognosis – Inability to identify familiar objects by touch alone.
- Ataxia – Impaired coordination of voluntary movements.
- Broca’s Aphasia – Retained ability to speak, but impaired language comprehension.
- Confabulation – Fabrication of false memories to fill in memory gaps.
- Dyskinesia – Uncontrolled, abnormal muscle movements.
- Dystonia – Sustained, repetitive muscle contractions leading to involuntary movements and abnormal postures.
| Condition | Cause | Signs & Symptoms | Diagnostics | Treatment | Key Concerns |
|---|---|---|---|---|---|
| Retinal Detachment | Risk factors include severe nearsightedness, history of cataract surgery, and family or personal history of retinal detachment. | Sudden increase in floaters or specks in vision, flashes of light, and a sensation of a curtain covering part of the visual field. | Clinical evaluation | Laser surgery or cryopexy (freezing treatment). | Can lead to permanent blindness if untreated. |
| Temporal Arteritis (Giant Cell Arteritis) | Unknown cause, but often associated with autoimmune inflammation of arteries. | One-sided temporal headache with tenderness or firmness over the temporal artery; may include sudden vision loss in one eye (amaurosis fugax) and scalp sensitivity on the affected side. | Elevated ESR (screening test). | Immediate corticosteroid therapy. | Untreated cases can lead to irreversible blindness. |
| Acute Angle-Closure Glaucoma | Sudden blockage of drainage channels in the eye, leading to increased intraocular pressure. | Sudden, severe eye pain with headache, nausea/vomiting, eye redness, excessive tearing, blurred vision, and halos around lights. | Tonometry to measure intraocular pressure. | Emergency—call 911. Immediate ophthalmologic intervention required. | Can cause permanent vision loss if not treated urgently. |
| Stroke (CVA) | Blockage (ischemic) or rupture (hemorrhagic) of a cerebral artery. | Sudden neurological impairment worsening over hours: blurred vision, slurred speech, one-sided limb weakness, hemianopsia, confusion. Symptoms depend on the location of infarct. | Brain imaging (CT, MRI), neurological assessment. | Emergency medical intervention—depends on stroke type (thrombolytics, surgery, rehabilitation). | Transient Ischemic Attack (TIA) resolves within 24 hours but signals increased stroke risk. |
| Actinic Keratosis | Chronic sun exposure—precursor to squamous cell carcinoma. | Small, rough, pink to reddish lesions that do not heal, commonly found on sun-exposed areas (cheeks, nose, neck, arms, chest). More frequent in light-skinned individuals. | Skin biopsy if needed. | Cryotherapy for isolated lesions; multiple lesions may require 5-fluorouracil cream. | If untreated, can progress to squamous cell carcinoma. |
| Hip Fracture | Common in individuals with osteoporosis or osteopenia. | Sudden onset of limping, guarding, and difficulty or inability to bear weight on the affected side. New hip pain (may radiate to the knee or groin). Leg may appear shorter or turned outward. | X-ray, MRI if needed. | Surgical intervention (hip replacement or fixation). | Major cause of morbidity and mortality in the elderly—20% of hip fracture patients die from complications (e.g., pneumonia). |
| Colorectal Cancer | Often develops from precancerous polyps. | Unexplained iron-deficiency anemia, rectal bleeding, hematochezia, melena, abdominal pain, or changes in bowel habits. Tenesmus (feeling of incomplete bowel movement), rectal pain, and narrow “ribbon-like” stools (suggests descending colon involvement). | Colonoscopy, stool tests, imaging. | Referral to gastroenterology for further evaluation and management. | Early detection improves survival rates. |
| Severe Bacterial Infections | Pneumonia, sepsis, pyelonephritis, bacterial endocarditis. | Atypical presentation in elderly: may be afebrile, have normal WBC count, experience sudden mental decline, new-onset incontinence, increased falls, inability to perform daily activities, and appetite loss. | Blood tests, cultures, imaging as needed. | Appropriate antibiotic therapy based on infection type. | Urinary tract infections (UTIs) are a common cause of sudden decline in older adults. |
| Multiple Myeloma | Cancer affecting plasma cells in the bone marrow. More common in older adults and 2-3 times more frequent in individuals of African descent. | Persistent bone pain, generalized weakness, increased risk of fractures. | CBC, fecal occult blood test (FOBT), chemistry panel, urinalysis. | Referral to a hematologist for specialized treatment. | Requires long-term management; can cause significant bone damage and kidney issues. |
Medications to Avoid in Older Adults (Beers Criteria)
| Drug Class | Medications to Avoid |
|---|---|
| Antihistamines | Diphenhydramine (Benadryl), Chlorpheniramine |
| Benzodiazepines | Short to intermediate-acting: Alprazolam (Xanax), Lorazepam (Ativan), Triazolam (Halcion) Long-acting: Diazepam (Valium), Clonazepam (Klonopin) |
| Antipsychotics | Thioridazine (Mellaril), Mesoridazine (Serentil) |
| Atypical Antipsychotics | Quetiapine (Seroquel), Olanzapine (Zyprexa) – Regular monitoring of BMI, lipids, TSH, and blood glucose is required. |
| Tricyclic Antidepressants (TCAs) | Amitriptyline (Elavil), Imipramine (Tofranil), Doxepin |
| Cardiac Medications | Increased risk of orthostatic hypotension |
| Alpha-Blockers | Terazosin, Clonidine – Higher risk of hypotension |
| Sulfonylureas | Glyburide, Chlorpropamide |
| NSAIDs | Increased risk of gastrointestinal bleeding |
| Mineral Oil, Proton Pump Inhibitors (PPIs) | Risk of aspiration pneumonia, increased risk of C. difficile infection in hospitalized patients, reduced absorption of calcium and magnesium |
| Sedative-Hypnotics | Zolpidem (Ambien), Eszopiclone (Lunesta) – Minimal sleep improvement with potential adverse effects |
| Antispasmodics | Dicyclomine (Bentyl), Scopolamine, Belladonna alkaloids |
| Other | Metoclopramide (Reglan) – Avoid except in gastroparesis; Sliding scale insulin – Not recommended due to risk of hypoglycemia |
Pediatrics
Newborn Characteristics
- Optimal visual range: 8–12 inches (distance from mother’s breast to eyes)
- Slight bluish tint in sclera, regardless of ethnicity
- Eyes are sensitive to light
- Protective blinking reflex present from birth
- Shows a preference for human faces
- Best hears high-pitched voices
- Responds to cries of other newborns
- Strong sense of smell
- Produces about six wet diapers daily
- Breastfed infants typically have around four stools per day
- Can lose up to 10% of birth weight in the first week but usually regain it by the second week
Behavioral Guidance
- Time-Out – Brief, structured separation to discourage unwanted behavior; child sits in a designated, non-stimulating, and safe area reserved solely for time-outs; use a timer for consistency.
- Suitable for ages 18–24 months and older
- Duration: 1 minute per year of age
Miscellaneous Insights
- Multi-system conditions often involve the skin, lymphatic system, and other organs, commonly due to viral infections.
- Growth milestones – Birth weight doubles by 6 months and triples by 12 months.
- Autism screening is recommended at 18 and 24 months.
- Age-appropriate responses may include resistance during medical examinations.
Warning Signs in Development
- 6 months – Absence of broad smiles or other warm, engaging expressions.
- 9 months – Lack of reciprocal interactions such as exchanging sounds, smiles, or facial expressions.
- 12 months – Does not respond to their name, absence of babbling, and no gestures like pointing, reaching, waving, or showing.
- 16 months – No spoken words.
- 24 months – Fails to produce meaningful two-word phrases that are not simply imitations or repetitions.
Primitive Reflexes
- Moro Reflex – Sudden movement or loud noise causes arms and legs to extend outward, then retract toward the body. Disappears by 16 weeks.
- Palmar Grasp – Fingers instinctively close around an object placed in the palm. Fades by 2-3 months.
- Babinski Reflex – Stroking the sole of the foot triggers toe fanning. Resolves by 6 months.
- Parachute Reflex – When placed on the stomach, the back arches and head lifts. Persists until 12 months.
- Tonic Neck Reflex – When the back is stimulated, the trunk and hips move toward the side of the stimulus. Vanishes by 9 months.
- Stepping Reflex – When held upright with feet touching a surface, the legs make a walking motion. Appears at 3-4 months, then returns at 12-24 months.
- Rooting Reflex – Turning of the head and sucking response when the cheek is stroked. Disappears between 6-12 months.
Speech Development Milestones
- 16-18 months – Speech is understood 16-25% of the time.
- 19-21 months – Comprehensibility increases to 50%.
- 2 to 2.5 years – Speech clarity reaches 75%.
- 3 to 4 years – Nearly 100% of speech is intelligible.
Tooth Development Timeline
- Incisors emerge first.
- Upper central incisors appear between 8-12 months.
- Lower central incisors erupt around 6-10 months.
- No teeth by 12 months? Seek a dental evaluation.
- Molars are the first permanent teeth to develop.
Growth and Milestones
At 2 Months:
- Lifts upper body with both arms while on tummy.
- Reacts to sounds.
- Smiles in response to others.
At 4 Months:
- Reaches for toys and objects.
- Smiles for enjoyment.
- Rolls from tummy to back.
At 6 Months:
- Sits upright, resembling the number 6.
- Rolls from back to tummy and back again.
At 8 Months:
- Transfers objects between hands after mastering sitting.
At 12 Months:
- Starts walking.
At 18 Months:
- Names single objects.
- Imitates adult tasks like an 18-year-old.
- Frequently says “no”.
At 2 Years:
- Forms two-word phrases.
- Understands and follows two-step instructions.
- Stacks two blocks.
- Walks upstairs with assistance.
At 3 Years:
- Pedals a tricycle.
- Constructs three-word sentences.
- Draws a circle.
- Builds a three-block tower.
- Foreskin remains difficult to retract until around age three.
At 4 Years:
- Copies a cross.
- Sketches a person with three body parts.
Clinic Checkups
2-3 Days After Birth
- Monitor for jaundice.
- Assess breastfeeding progress.
- Track weight fluctuations.
- Review newborn screening results.
- Evaluate maternal health.
- Provide infant care education.
1 Week Checkup
- Confirm weight gain.
- Observe elimination habits.
- Discuss sleep and wake patterns.
- Assess parent-infant bonding.
- Reassess newborn screening status.
- Check for skin conditions (milia, port-wine stain, nevus simplex, Mongolian spot).
- Examine fontanelles (posterior closes ~3 months; anterior closes ~9-18 months).
- Inspect eyes (temporary crossing normal until ~2 months; hypertelorism = widely spaced eyes).
- Low-set ears could suggest kidney abnormalities.
- Address hearing concerns early—intervene by 6 months if necessary.
- Palpate clavicles for fractures; if broken, handle infant as a unit.
- Check femoral pulses to rule out coarctation of the aorta.
- Examine umbilical cord, may require silver nitrate treatment.
- Inspect genitalia.
- Fat pads on feet can mimic flat feet (pes planus).
- Spine check—look for neural tube defects; tuft of hair may indicate need for ultrasound.
Hyperbilirubinemia (>5 mg/dL)
- Due to immature liver struggling to process bilirubin.
- Results from red blood cell breakdown, causing bilirubin deposits in skin.
- Risk of kernicterus (bilirubin-induced brain damage).
Infant Nutrition
- Exclusive breastfeeding recommended for the first six months.
- Introduce solid foods around 4-6 months.
- Start with single-ingredient, iron-fortified rice cereal.
- Whole cow’s milk should be introduced at 12 months.
- Breastfed infants require vitamin D supplementation.
Evaluation & Screening
- Eyes: Check red reflex, visual acuity
- Amblyopia: Most common cause of vision loss in children
- Corneal light reflex & cover/uncover test
- Strabismus: Refer to ophthalmology if present after 3 months
- 20/20 vision typically achieved by age 6
- Ears: Monitor for speech delays
- Heart:
- Murmurs are common; heart rate decreases as the heart grows
- Blood pressure screening starts at age 3
- Gastrointestinal: Umbilical hernia—easily reducible
- Musculoskeletal: Screen for hip dysplasia
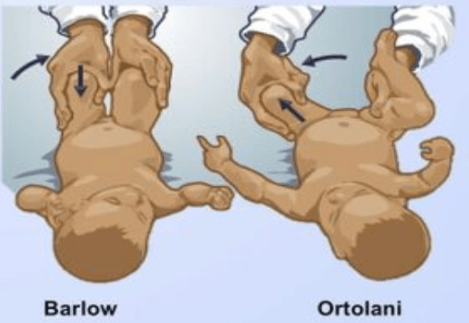
- Barlow test: Checks if the femoral head moves toward the buttocks
- Ortolani test: Detects hip dislocation
- Galeazzi test: Assesses leg length discrepancy (hip dysplasia indicator)
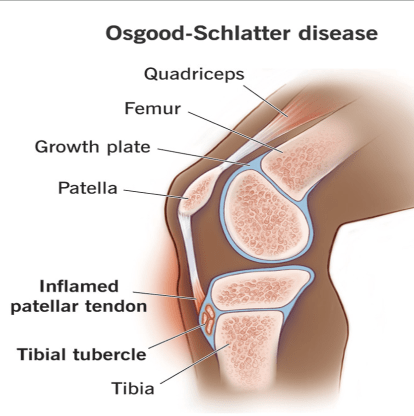
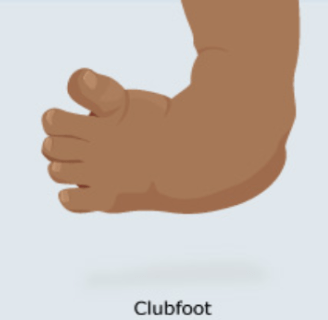
- Clubfoot (talipes equinovarus): Requires orthopedic evaluation
- Metatarsus adductus:
- If feet can be moved to midline, encourage 10 stretches per diaper change
- If not, refer to orthopedics

Musculoskeletal Evaluation
- Scoliosis: Highest risk period is puberty
- Spinal curvature of 10 degrees is diagnostic
- Adams forward bend test for screening
- Scoliosis series (full-length PA/Lateral X-rays) for assessment
- Younger age at diagnosis = higher risk for progression
Managing Vomiting
- Assess weight and growth trajectory in all children with vomiting
- Rehydrate using Pedialyte to restore fluids and electrolytes
Adolescent Development
- Identity vs. Role Confusion
Early Adolescence (10-14 years)
- Egocentric mindset, concrete thinking, early moral dilemmas
- Evolving sexual identity, heightened focus on body image
- Emotional distancing from parents, self-exploration, peer-driven identity
- Early experimentation with risky behaviors (e.g., substance use)
- Engage in dangerous activities—emphasize safety measures like seatbelts
Middle Adolescence (15-17 years)
- Peer influence outweighs parental guidance
- Expanding abstract reasoning, belief in personal invincibility, strong verbal skills
- Tendency toward black-and-white thinking in ideological beliefs (e.g., political, religious)
- Further emotional independence, increased peer reliance
- Higher risk-taking behaviors (e.g., smoking, alcohol use), early career planning
Late Adolescence (18-21 years)
- Greater abstract reasoning, improved impulse regulation
- Continued refinement of personal identity and ideology (acceptance or rejection)
- Increased emotional and social autonomy, deepening intimate relationships
- Development of career goals and financial self-sufficiency
Tanner Stages of Puberty
Stage 1 (Prepubertal)
- No visible secondary sexual characteristics; body appears childlike
Stage 2 (Pubertal Onset)
- Girls: Breast budding (thelarche), sparse pubic hair (pubarche)
- Boys: Testes and scrotum begin enlarging
- General Rule: Breast budding to first menstrual period ≈ 2 years
- Marks the official start of puberty
Stage 3 (Mid-Puberty)
- Growth spurt begins (fastest growth period)
- Girls: Breasts enlarge into a single mound
- Boys: Penis lengthens
- Gynecomastia may develop in boys (temporary); overweight boys may show pseudogynecomastia
Stage 4 (Late Puberty)
- Girls: Menstruation typically begins
- Most girls reach adult height about a year after their first period
- Breast areola becomes elevated, forming a secondary mound
- Boys: Penis widens, testes enlarge further, scrotal skin darkens and develops more rugae
Stage 5 (Maturity)
- Fully developed adult sexual characteristics
Key Mnemonics:
- Boys: “Balls → Long → Wide” (Testes enlarge → Penis lengthens → Penis widens)
- Girls: “Boobs – Bud → One → Two” (Breast bud → Single mound → Secondary mound)
Puberty Timing:
- Girls: Normal onset 8-13 years
- Before 7-8 years: Early puberty (often idiopathic, refer to pediatric endocrinologist)
- After 13 years: Delayed puberty (causes may include low body weight, eating disorders, intense athletics, or genetics)
- Boys: Normal onset 9-14 years
- Before 9 years: Early puberty (refer to pediatric endocrinologist)
Vaccination Guidelines
General Vaccine Timing
- Can be administered up to 4 days early without issue
- 5+ days early is considered invalid
Hepatitis A
- Recommended for all children at 1 year
- Two-dose series given at least 6 months apart
Hepatitis B
- Three-dose series:
- At birth (0 months)
- 1-2 months
- 6 months
DTaP (Diphtheria, Tetanus, Pertussis) – for children under 7
- Minimum starting age: 6 weeks
- Five-dose schedule:
- 2 months
- 4 months
- 6 months
- 15-18 months
- 4-6 years
Tdap (for ages 7+)
- First dose at 11-12 years
- Td booster every 10 years
- Given during each pregnancy (3rd trimester)
Hib (Haemophilus influenzae type B)
- 4-dose schedule:
- 2 months
- 4 months
- 6 months
- 12-15 months
- If unvaccinated and older than 15 months, a single dose is given
Pneumococcal Vaccine (PCV13)
- 4-dose schedule:
- 2 months
- 4 months
- 6 months
- 12-15 months
- Certain high-risk groups also require PCV23
Polio (Inactivated Poliovirus Vaccine – IPV only)
- 4-dose schedule:
- 2 months
- 4 months
- 6-18 months
- 4-6 years
- Contraindicated in individuals allergic to neomycin, streptomycin, or polymyxin B
- Oral polio vaccine (live virus) is no longer used
Influenza Vaccine
- Annual vaccination for everyone
Meningococcal Conjugate Vaccine (MCV4)
- First dose at 11-12 years
- Booster dose at 16 years
HPV-9 (Human Papillomavirus Vaccine)
- Recommended starting at age 9-14
- Two-dose series:
- 0 months
- 6-12 months later
- Not recommended during pregnancy but safe for breastfeeding
Live Vaccines
- Require replication to build immunity, often causing fever or rash
- Not recommended before 12 months of age
MMR (Measles, Mumps, Rubella)
- First dose: 12-15 months
- Second dose: 4-6 years
Varicella (Chickenpox)
- First dose: 12-18 months
- Second dose: 4-6 years
- If receiving the first dose at 13 years or older, a two-dose series is required, spaced at least one month apart
- Not safe for individuals allergic to neomycin or gelatin
Spacing Requirement
- Must wait at least 28 days between two live vaccines
Vaccine Side Effects
- Types of Reactions:
- Localized: Redness, swelling at the injection site
- Systemic: Fever, general discomfort
- Allergic: Rare but possible severe reactions
- Fainting (Syncope): Common with HPV, MCV4, and Tdap vaccines
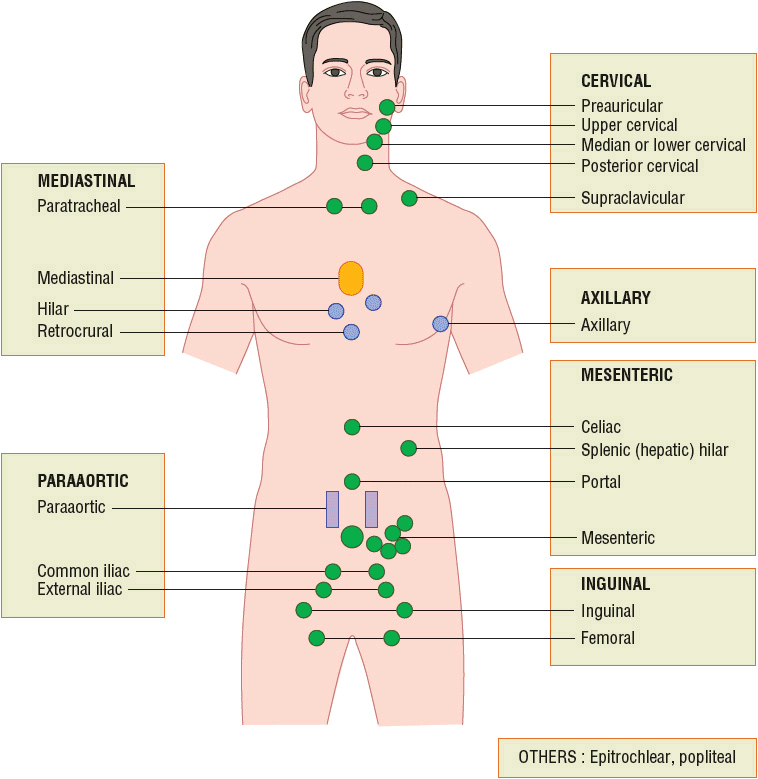
Lymph Node Guidelines
- General Enlargement Threshold: >10mm
- Exceptions:
- Epitrochlear: >5mm
- Inguinal: >15mm
- Cervical: >20mm
Fluid Loss & Hydration Status
| Category | Mild | Moderate | Severe |
|---|---|---|---|
| Pulse | Normal | Fast | Rapid and weak |
| Blood Pressure | Normal | Normal to low | Low |
| Respiration | Normal | Deep, increased rate | Deep, increased rate |
| Mucous Membranes | Slightly sticky | Dry | Severely dry (parched) |
| Anterior Fontanel | Normal | Sunken | Deeply sunken |
| Eyes | Normal | Sunken | Very sunken |
| Skin Turgor | Normal | Decreased elasticity | Tenting (skin remains elevated) |
| Skin Temperature | Normal | Cool | Cool and mottled |
| Urine Output | Normal | Reduced | Absent |
| Systemic Signs | Thirsty | Irritable | Lethargic |
Are they able to keep liquids down?
Undeveloped Testicular Descent
Increased likelihood of testicular cancer
Cryptorchidism – failure of testes to descend
Retractile testes – shifts between the scrotum and inguinal canal
Specialist referral if not descended by 6 months
THREADWORM INFECTION
Enterobiasis
Use Scotch tape test in the morning to detect eggs
o Worms emerge at night to deposit eggs around the anus
o Test multiple mornings as eggs aren’t laid daily
Symptoms typically appear 4-8 weeks post-exposure
Managed with Albendazole
BIRTH-RELATED HEART CONDITIONS
Signs of Harmless Murmurs:
- Intensity below grade 2
- Becomes quieter when sitting compared to lying down
- Not continuous throughout systole
- Minimal sound transmission
- Has a musical or vibratory tone
Indicators of Concerning Murmurs:
- Intensity above grade 3
- Heard throughout systole (holosystolic)
- Most prominent at the left upper sternal border (LUSB)
- Harsh or blowing in nature
- Presence of systolic clicks
- Audible during diastole
- Louder when standing upright
- Accompanied by gallop rhythm
- Friction rub present

| Condition | Cause | Signs & Symptoms | Diagnostics | Treatment | Concerns |
|---|---|---|---|---|---|
| Jaundice | Physiologic jaundice occurs without liver disease; other causes may involve liver dysfunction | Yellowing begins on the face and spreads downward to the trunk and limbs | Encourage breastfeeding every 2-3 hours | Physiologic jaundice appears after 24 hours of life; jaundice in the first 24 hours may indicate liver disease | |
| Galactorrhea | Maternal hormonal influences | Breast milk secretion without lactation, typically starts on day 3-4 of life. Breast engorgement resolves within 2 months | No intervention needed unless symptomatic | Some cultures may view this condition negatively; consider family concerns | |
| Chlamydial (Inclusion) Conjunctivitis | Exposure to Chlamydia | Symptoms appear 5-14 days after birth; bilateral eyelid swelling, chemosis, and mucoid discharge | Oral erythromycin for 2 weeks due to risk of pneumonia | Routine STI screening in the third trimester helps prevent transmission | |
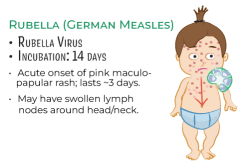
| Rubella (German Measles, 3-Day Measles) | Rubella virus | Fever, sore throat, nasal discharge, malaise, diffuse maculopapular rash lasting ~3 days. Posterior cervical & postauricular lymph node swelling appears 5-10 days before rash. Arthralgia in 25% of cases. | Lab-confirmed Rubella IgM | Reportable disease; droplet precautions; public health determines return to school. Mask patient until home. Prevent with MMR vaccine. | Teratogenic virus (dangerous in pregnancy) |
| Rubeola (Measles) | Rubeola virus | Fever, nasal discharge, cough, conjunctivitis (clear, copious discharge), photophobia, Koplik spots, maculopapular rash spreading from head downward, pharyngitis | Lab-confirmed Rubeola IgM | Reportable disease; prevent with MMR vaccine | Highly contagious, severe complications possible |
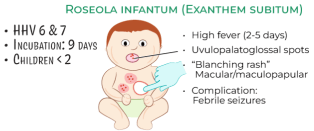
| Roseola Infantum | Human Herpesvirus 6 (HHV-6) | High fever (2-4 days), followed by a pink maculopapular rash on the body (sparing the face) | Self-limiting | Most common in infants 7-13 months old | |
| Erythema Infectiosum (Fifth Disease) | Parvovirus B19, spreads via respiratory secretions | “Slapped cheek” rash with lacy maculopapular rash on the body | Self-limiting | Can cause miscarriage if contracted by a pregnant woman, especially in the first trimester | |
| Hand, Foot, and Mouth Disease | Coxsackie A Virus | Fever, malaise, sore mouth, anorexia; 1-2 days later, painful oral lesions; may also cause conjunctivitis & pharyngitis; lasts 2-7 days | Prevent dehydration; symptoms resolve in 2-3 days | Differentiate from herpangina, which has only mouth ulcers | |
| Kawasaki Disease | Inflammation of coronary arteries (vasculitis) | Fever for 5+ days plus conjunctival injection, polymorphous rash, inflamed lips/oral mucosa (strawberry tongue), swollen hands & feet, cervical lymphadenopathy | CBC, ESR/CRP, ALT/AST, UA, throat culture, echocardiogram | IV immune globulin, high-dose aspirin; daily aspirin for 2 months | More common in boys than girls; risk of coronary aneurysms |
| Condition | Cause | Signs & Symptoms | Diagnostics | Treatment | Concerns |
|---|---|---|---|---|---|
| Mononucleosis | Epstein-Barr virus | Fever, shaggy purple-white exudative pharyngitis, fatigue, widespread lymph node swelling, liver & spleen tenderness (sometimes enlarged), maculopapular rash in 20% (rarely petechial) | Monospot test (heterophile antibody test) | Avoid Amoxicillin—can cause a morbilliform rash | More symptomatic in teenagers & adults than young children |
| Iron Deficiency Anemia | Low iron stores at birth, introduction of a low-iron diet in late infancy or early toddler years | Common between 12-30 months | Microcytic, hypochromic anemia with increased RDW | Lead toxicity can mimic iron deficiency—symptoms include abdominal pain, fatigue, and irritability | |
| Croup (Laryngotracheobronchitis) | Viral infection | Barking cough, may have stridor | Supportive care; single dose of Decadron (long half-life of 72 hours) | ||
| Foreign Body Aspiration | Mechanical obstruction | Inspiratory stridor | Chest X-ray (2 views) | Urgent removal; refer to ER if needed | Foreign object in the nose may cause unilateral purulent nasal discharge |
| Peritonsillar Abscess | Bacterial infection | Muffled “hot potato” voice, difficulty swallowing, trismus (jaw stiffness), uvula deviates to the opposite side, possible stridor | Maintain airway, urgent ENT consult, antibiotics, possible surgical drainage | Can require hospital admission for airway monitoring | |
| Acute Epiglottitis | Haemophilus influenzae | Dysphagia, drooling, stridor, hoarseness, sore throat, fever, “thumb sign” on imaging | Airway stabilization, emergency ENT consult | Can rapidly progress to airway obstruction | |
| Bronchiolitis | Respiratory Syncytial Virus (RSV) | Fever, cough, increased respiratory rate, “happy wheezer”; affects ages 3 months – 3 years; wheezing may persist up to 3 weeks | Supportive care—hydration & oxygen; no bronchodilators or steroids | Most severe in infants under 1 year; Synagis (palivizumab) available for high-risk cases | |
| Wilms Tumor | Nephroblastoma | Painless abdominal mass extending from the flank to the midline; avoid deep palpation to prevent rupture | Ultrasound | Refer for oncology evaluation | More common in Black females; peak incidence at ages 2-3 years |
| Encopresis | Involuntary stool passage due to chronic constipation | Stool retention leads to loss of normal sensation to defecate | Laxatives (MiraLAX) for initial clearing; behavior training (sit on the toilet for 5 min, 2-3x daily after meals); increase fiber & fluids | More common in boys; assess school bathroom access; in girls, consider screening for sexual abuse |
| Condition | Cause | Signs & Symptoms | Diagnostics | Treatment | Concerns |
|---|---|---|---|---|---|
| ADHD | Neurodevelopmental disorder affecting attention, impulse control, and activity levels | Three types: Combined Type (both inattentive & hyperactive/impulsive); Predominantly Inattentive; Predominantly Hyperactive/Impulsive | Symptoms must: (1) Appear before age 12, (2) Persist for over 6 months, (3) Be present in at least two settings (e.g., home & school) | Diagnosis via behavioral rating scales (e.g., Vanderbilt, Conners’ Rating Scale, Child Behavior Checklist) | If coexisting conditions exist, referral may be needed. Typically managed with Schedule II medications |
| Asthma | Chronic inflammatory airway disease | Symptoms similar to adults | Same diagnostic criteria as adults, but children may benefit more from leukotriene receptor antagonists like Singulair (1 in 3 cases) | Nebulizer or spacer-assisted inhalers | Most common chronic disease in children |
| Pneumonia | Typically viral, but if bacterial, Streptococcus pneumoniae is most common | Increased respiratory rate is the most sensitive finding | Chest X-ray, CBC | High-dose Amoxicillin (90 mg/kg/day) | |
| Cystic Fibrosis | Autosomal recessive disorder affecting sodium and chloride transport | Thick mucus causes recurrent sinus & lung infections, pancreatic duct blockage (leading to weight loss & greasy stools) | Sweat chloride test | Multisystem disease—affects pulmonary, GI, and sweat glands | Most common in individuals of European descent |
| Leukemia | Most common childhood cancer | Evening fevers, easy bruising, frequent nosebleeds, bone pain, recurrent infections, lymphadenopathy, fatigue, poor appetite, hepatosplenomegaly | Lab findings: ↓ WBC, ↓ H/H, ↓ Platelets. Peripheral smear: Malignant cells. Bone marrow biopsy: Blast cell infiltration | Most common ages 2-8. Acute Lymphoblastic Leukemia (ALL) = 77%; Acute Myeloid Leukemia (AML) = 11% | |
| Pyloric Stenosis | Hypertrophy of the pyloric muscle causing gastric outlet obstruction | Projectile, nonbilious vomiting; most common in first-born males. Olive-shaped mass palpable in RUQ | Abdominal ultrasound | Surgery | Usually appears between 4-6 weeks of age. Differential: GERD, milk protein intolerance, intestinal obstruction |
| Gastroesophageal Reflux (GER) | Immature lower esophageal sphincter (LES) until ~9-12 months | Frequent regurgitation (>30 times/day in healthy infants); GERD indicated by irritability during reflux episodes | Red flags: Choking or coughing while eating, forceful vomiting, GI bleeding, poor weight gain, refusal to eat, abnormal bowel habits, abdominal tenderness, fever | Typically managed with feeding adjustments (small, thickened feedings, hypoallergenic or soy-based formula trial). Continue breastfeeding. Avoid prone sleeping | Distinguish between GER (normal) and GERD (pathological). Watch for red flag symptoms |
| Intussusception | Intestinal telescoping causing obstruction | Sudden episodes of crampy, progressive abdominal pain. Child may act normal between episodes. “Current jelly” stools and sausage-shaped mass in abdomen | KUB X-ray, ultrasound | Barium enema (diagnostic & therapeutic), surgical intervention if needed | Typically occurs in children under age 2 |
| Condition | Cause | Signs & Symptoms | Diagnostics | Treatment | Concerns |
|---|---|---|---|---|---|
| Legg-Calvé-Perthes Disease | Avascular necrosis of the proximal femoral head | Limping, hip and/or knee pain | Trendelenburg’s Sign: Standing on the affected side causes a pelvic tilt. Hip X-ray (AP & frog-leg views) | Referral to orthopedics | Typically seen in children ages 3-12; more common in males than females |
| Slipped Capital Femoral Epiphysis (SCFE) | Displacement of the femoral head from the hip joint | Hip/knee pain for weeks to months, intermittent limp | Trendelenburg’s Sign: Pelvic tilt when standing on the affected side. Hip X-ray (AP & frog-leg views) | Immediate orthopedic referral for surgical fixation | Frequently occurs in adolescents |
| Fragile X Syndrome | Genetic disorder (FMR1 mutation) | Males: Large forehead, ears, prominent jaw, macroorchidism (large testicles), tall stature, behavioral challenges, eye contact avoidance. Females: Milder symptoms, fewer physical features | Genetic testing for carrier status | Supportive therapy | Leading known genetic cause of autism |
| Klinefelter Syndrome (XXY male) | Extra X chromosome in males | Low testicular volume, breast & hip enlargement, infertility, developmental delays (especially in language) | Genetic testing for carrier status | Supportive management | |
| Turner Syndrome (XO female) | Missing or partially missing X chromosome | Short stature (<5 ft.), wide webbed neck, broad shield-shaped chest, absent menstruation, infertility, high-arched palate, low-set ears, hand/foot edema. Mosaic Turner’s presents with milder features | Genetic testing; High rate of pregnancy loss | Hormonal therapy, supportive care |