Orthopedic Assessments
Drawer Test
Evaluates knee ligament integrity and detects instability

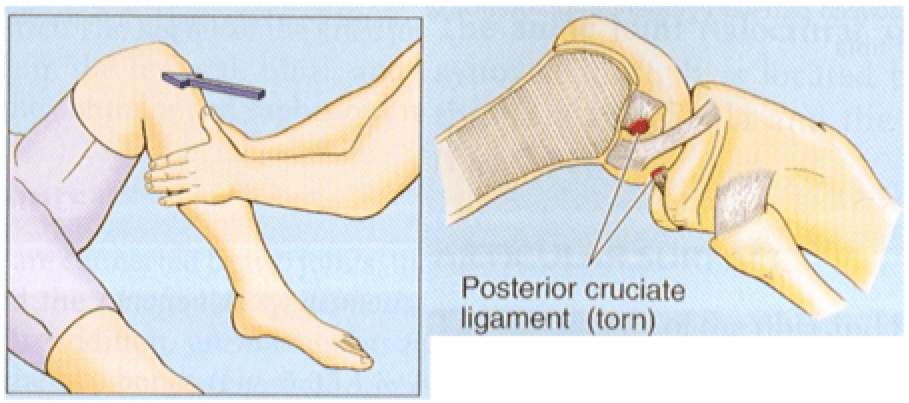
McMurray Test
Detects medial meniscus tear; a “click” is felt when the knee is manipulated while rotating the ankle.

Lachman Test
Highly sensitive for ACL injury, more reliable than the drawer test.
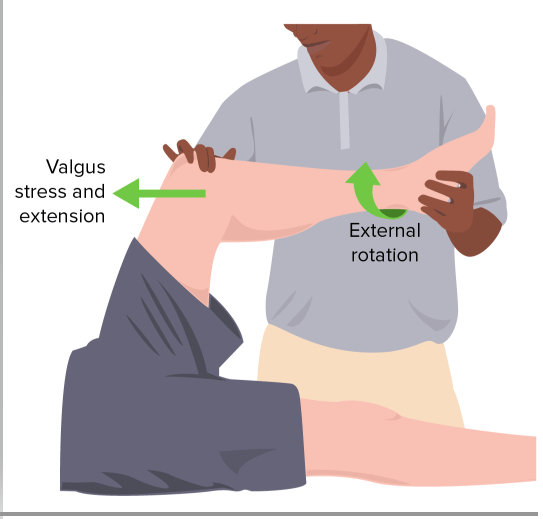
Collateral Ligament Assessment
Increased laxity indicates ligament damage.
- Valgus Stress Test – Identifies medial collateral ligament (MCL) injury.
- Varus Stress Test – Detects lateral collateral ligament (LCL) damage (Varus = Lateral).

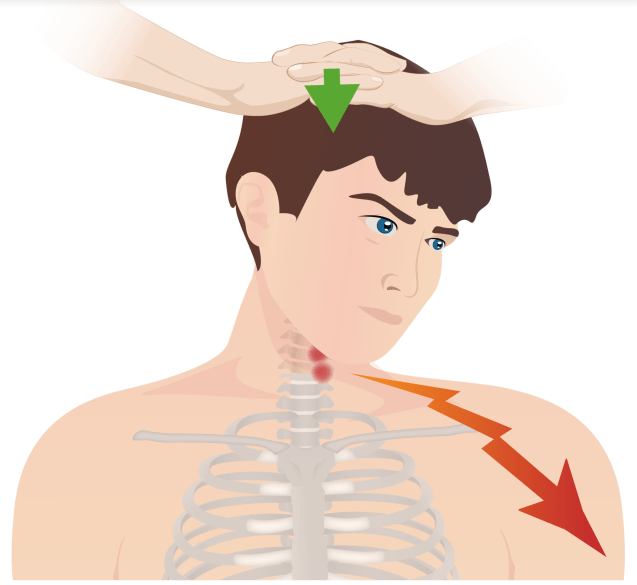
Spurling’s Maneuver
Also known as the Foraminal Compression Test, Neck Compression Test, or Quadrant Test
- Performed by extending the neck, rotating the head, and applying downward pressure.
- A positive result reproduces radicular pain radiating into the arm on the same side as head rotation.
- Diagnostic Value:
- 92% sensitivity, 95% specificity
- Low sensitivity makes it ineffective for screening, but its high specificity helps confirm a diagnosis.
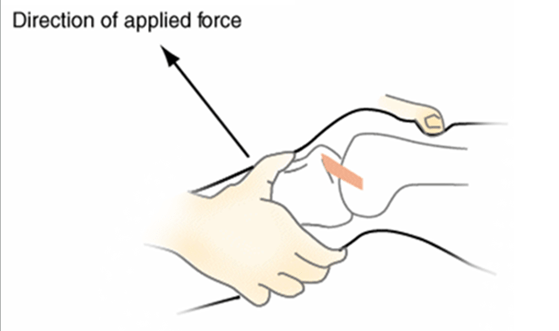
Finkelstein’s Maneuver
Used to diagnose De Quervain’s tenosynovitis, caused by inflammation of the tendons at the base of the thumb.
- Positive test: Pain occurs with ulnar deviation of the wrist while the thumb is tucked into the fist.

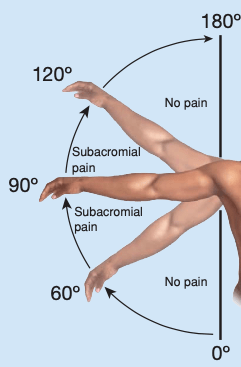
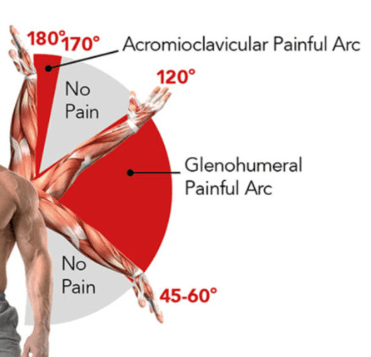
Shoulder Impingement Syndrome
- Pain occurs when the hand is at or above shoulder height, typically felt in the lateral shoulder region.
- Common discomfort when reaching overhead, such as grabbing an item from a pantry or closet.
- Painful Arc Test is used for assessment.
Rotator Cuff Tear
- Pain in the lateral deltoid region.
- Weakness and loss of strength in external rotation or abduction.
- Often worsens at night, disrupting sleep.
Adhesive Capsulitis (Frozen Shoulder)
- Anterior shoulder pain with joint stiffness.
- Noticeable restriction in movement, particularly external rotation and abduction.
- Frequently associated with diabetes.
AC Joint Osteoarthritis (AC OA)
- Tenderness over the AC joint.
- Presence of osteophytes and joint space narrowing.
Extrinsic Shoulder Pain
- Cervical Nerve Root Compression
- Neck range of motion (ROM) triggers pain? → Indicates a cervical issue.
- Spurling’s test can help confirm.
- Other Causes
- Myocardial ischemia
- Splenic injury
- Ectopic pregnancy
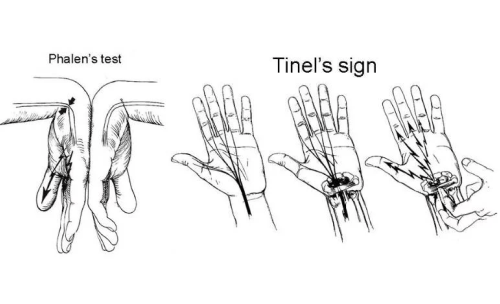
Phalen’s Test
- Maximally flex the wrist and hold for 60 seconds.
Tinel’s Sign
- Tap over the transverse carpal ligament.
➤ Associated Symptoms
- Pain
- Numbness (Anesthesia)
- Tingling (Paresthesia)
Physical Activity & Injury Management
First 48 Hours:
- Avoid exercise
- Apply cold therapy
R.I.C.E. Protocol:
- Rest, Ice, Compression, Elevation
After 48 Hours:
- Begin isometric exercises
Tendonitis: Causes, Symptoms, and Management
➤ Overview:
- Microtears in tendons lead to inflammation and pain
- Typically caused by repetitive strain, microtrauma, or overuse
- Develops gradually
- Sharp pain when pressure is applied to the tendon
- Reduced range of motion (ROM) due to stiffness and discomfort
- R.I.C.E. therapy recommended
Common Types of Tendonitis:
Supraspinatus Tendonitis (Rotator Cuff Tendonitis)
- Shoulder pain with specific movements (e.g., raising arm, reaching behind the back)
- Clicking sensation when lifting the arm overhead
- Localized tenderness in the front of the shoulder
- Common causes: Swimming, throwing, pitching, raking, washing windows/cars
- Often associated with bursitis
Epicondylitis (Elbow Tendonitis)
Lateral Epicondylitis (Tennis Elbow):
- Gradual onset of pain on the outer elbow, extending into the forearm
- Overuse injury (e.g., twisting or gripping—opening jars, shaking hands)
- Pain worsens with wrist extension
- Weak grip strength
Medial Epicondylitis (Golfer’s Elbow):
- Inner elbow pain that develops gradually
- Higher risk in: Golfers, bowlers, baseball players
- Reduced grip strength
- 95% of cases resolve without surgery
Additional Considerations:
- Rest while maintaining some joint mobility
- Possible complication: Ulnar nerve neuropathy
- Numbness/tingling in the pinky & ring finger
- Hand weakness, potential “claw hand” deformity
- Treatment options: TCAs, gabapentin, phenytoin, pain management
Tenosynovitis (Wrist Tendonitis):
- Pain, swelling, reduced ROM, and muscle weakness
Lower Back Pain: Causes, Symptoms, and Management
➤ Common Causes:
- Typically results from soft tissue inflammation, sciatica, sprains, muscle spasms, or herniated discs
- Most common affected areas: L4-L5 to S1 (lumbar hinge) and C6-C7 (cervical region)
- 90% of cases resolve within a month
Risk Factors:
✔ Aging
✔ Overuse or excessive activity
✔ Obesity
✔ Degenerative joint disease (DJD)
Typical Symptoms:
- Stiffness, muscle spasms, reduced range of motion (ROM)
- Early lumbar radiculopathy may present as diminished deep tendon reflexes (DTRs)
Red Flags for Further Evaluation:
✔ Significant trauma history or signs of infection
✔ Suspected cancer metastasis (new-onset back pain in individuals over 50)
✔ Possible spinal fracture risk (osteoporosis, chronic steroid use)
✔ Spinal stenosis suspicion (rule out ankylosing spondylitis)
✔ Worsening symptoms despite treatment
Neurological Exam Findings:
✔ Loss of posterior tibial reflex (L5)
✔ Loss of Achilles tendon reflex (L5-S1)
✔ MRI recommended for further assessment
Treatment Approach (Based on Cause):
Uncomplicated Cases:
- NSAIDs and warm compresses for muscle spasms
- Muscle relaxants if needed
- Core and abdominal strengthening after acute phase
- Avoid prolonged bed rest (prevents deconditioning)
Spinal Stenosis:
- Pain relief when sitting or bending forward
Herniated Disc:
- Feels better when standing
Potential Complication:
- Cauda equina syndrome (medical emergency)
Clinical Assessment:
✔ Inspection & palpation
✔ Check reflexes, muscle strength, sensation, and gait
✔ Straight leg raise test for radiculopathy
✔ Waddell’s Sign: Exaggerated pain response during examination (suggests non-organic pain)
Ottawa Guidelines for Sprains
✔ Grade 1 (Mild):
- Slight ligament stretching with minimal damage
- Joint remains stable
- Able to bear weight and walk
✔ Grade 2 (Moderate):
- Partial ligament tear
- Visible bruising, moderate swelling, tenderness on palpation
- Painful weight-bearing with mild to moderate joint instability
- Consider X-ray or specialist referral
✔ Grade 3 (Severe):
- Complete ligament rupture leading to joint instability
- Inability to bear weight or walk at least four steps
- Tenderness along the posterior malleolus
- Severe pain, extensive bruising, and resistance to foot movement
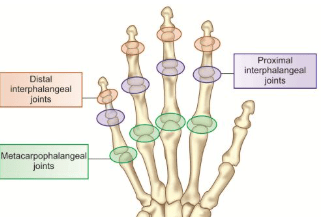
Rheumatoid Arthritis (RA) vs. Osteoarthritis (OA)
| Characteristic | Rheumatoid Arthritis (RA) | Osteoarthritis (OA) |
|---|---|---|
| Primary Joints Affected | Hands; metacarpophalangeal (MCP) joints | Weight-bearing joints, carpometacarpal (CMC), distal interphalangeal (DIP) joints |
| Heberden’s Nodes | Absent | Usually present |
| Joint Characteristics | Soft, warm, tender | Bony, hard |
| Lab Findings (RF, CCP, ESR, CRP) | Usually positive | Typically negative |
Sports Participation Assessment
Cardiovascular Screening: A Key Aspect of Pre-Participation Physicals
- Athletes under 35: Most cardiac-related deaths stem from congenital abnormalities
- Hypertrophic cardiomyopathy is a primary concern
- Athletes over 35: More likely to experience atherosclerotic coronary artery disease (CAD)
- Cardiac History Review:
- Previous episodes of chest pain, syncope
- Shortness of breath or fatigue during exertion
- History of heart murmur or high blood pressure
- Family history of early cardiac death or disease before age 50
Cardiovascular Physical Exam:
- Precordial auscultation in both supine and standing positions
- Femoral pulse assessment to rule out aortic coarctation
- Blood pressure measurement while sitting and standing
Medical Considerations for Athletes:
- Hypertension: Avoid beta-blockers (can suppress heart rate response) and diuretics (increase dehydration risk)
- Innocent murmurs: Generally safe but require cardiology evaluation
- Valvular Conditions:
- Aortic stenosis & mitral stenosis: Participation depends on severity
- Mitral regurgitation: Often due to rheumatic fever, endocarditis, or calcifications—activity allowance varies based on severity and ventricular size
- Mitral valve prolapse: Most common valvular issue, often seen with pectus excavatum; play is permitted if symptom-free
- Hypertrophic cardiomyopathy: A leading cause of sudden cardiac death; midsystolic murmur increases in intensity when standing
- Individuals with ICDs: Must be aware of potential risks
Congenital Defects & Sports Eligibility
- Atrial/Septal Defects:
- If surgically repaired with minimal residual dysfunction, full participation is allowed
- Unrepaired cases require evaluation; easy fatigue may indicate an atrial septal defect
- Children can present anywhere from asymptomatic to heart failure
- Common Murmurs & Findings:
- Still’s murmur: Has a characteristic buzzing quality
- S2 split: Sometimes found in uncorrected atrial septal defects
- Sinus arrhythmia: Not a concern—athletes are encouraged to play
Special Considerations:
- Down syndrome: Cervical spine X-ray required before participation due to the risk of atlantoaxial instability (AAI)
Clinical Insights & Key Concepts
Fractures & Bone Injuries:
- Pathological fractures: Can be linked to conditions like osteosarcoma or osteoporosis
- Stress fractures: Result from repetitive strain; typically require six weeks to heal
- Contusions: Bone injury without an actual fracture
Soft Tissue Injuries:
- De Quervain’s Tenosynovitis: Characterized by dorsal thumb pain—common in individuals who frequently use their fingers
- Strains: Involve muscle damage
- Sprains: Result from ligament injuries
Spinal & Neurological Concerns:
- Cauda equina syndrome: A serious condition caused by spinal cord compression
Preventive Care & Risk Factors:
- Vitamin D supplementation is advised for all adults over 50
- Ankle sprain risk factors:
- Poor physical conditioning
- Wearing improper footwear
- Skipping warm-up exercises before activity
Imaging Modalities & Their Uses
X-rays – Best for detecting bone fractures, osteoarthritis (OA), metallic objects, and other dense structures
MRI (Magnetic Resonance Imaging) – Gold standard for evaluating cartilage, meniscus, tendon, and ligament injuries
- Contraindications: Not suitable for individuals with metal implants, pacemakers, or aneurysm clips
CT (Computed Tomography) Scan – More cost-effective than MRI
- Useful for assessing masses, trauma-related injuries, fractures, and internal bleeding
- Produces detailed 3D images
Hook Maneuver
A diagnostic test used to assess distal biceps tendon integrity by attempting to “hook” the tendon with a finger.
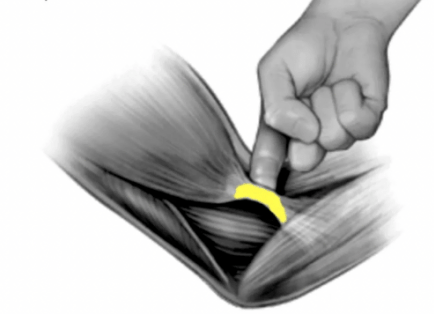
Biceps Tendon Rupture
A biceps tendon rupture occurs when the tendon detaches from the bone, leading to pain, weakness, and a visible deformity. It can be partial or complete and commonly affects the proximal or distal biceps tendon.

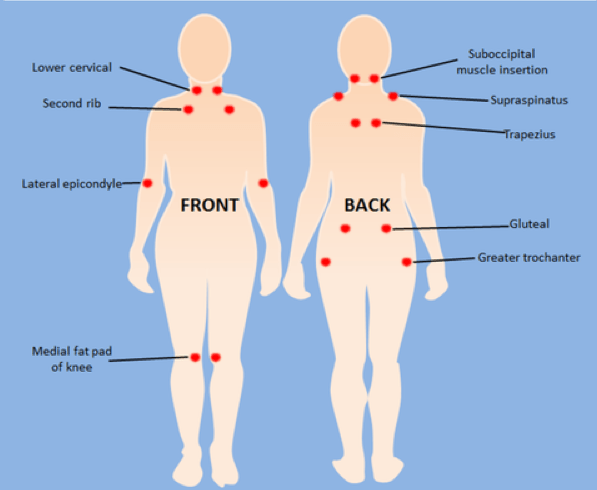
Fibromyalgia
✔ Underlying cause remains unclear
✔ Occurs 4 to 7 times more frequently in women
✔ Higher prevalence among individuals with autoimmune conditions
✔ Characterized by widespread musculoskeletal pain, fatigue, and cognitive disturbances (“fibro fog”)
Diagnosis:
- Identified by the presence of at least 11 out of 18 specific tender points
- Pressure should be applied until nail beds blanch
Management & Treatment:
- Physical activity focused on enhancing flexibility
- Trigger point injections may provide relief
- Medication options:
- Acetaminophen & NSAIDs for pain management
- Trazodone & antidepressants for sleep disturbances and mood stabilization
- Antiepileptic drugs for neuropathic pain
Orthopedic Terminology
✔ Abduction (Varus) – Motion that moves a limb away from the body’s midline
✔ Adduction (Valgum) – Motion that brings a limb toward the body’s midline
| Condition | Cause | Signs & Symptoms | Diagnostics | Treatment | Concerns |
|---|---|---|---|---|---|
| Navicular (Scaphoid) Fracture | Fall on an outstretched hand | Pain and tenderness in the “snuffbox” region; worsens with gripping or squeezing | X-ray may appear normal initially; repeat in 2 weeks | Immobilize with a thumb spica splint; refer to hand specialist | Risk of avascular necrosis and nonunion |
| Colles Fracture | Distal radius fracture from a fall | “Dinner fork” deformity; most common wrist fracture | X-ray | Immobilization or surgical intervention based on severity | Possible long-term stiffness or arthritis |
| Hip Fracture | Falls | Sudden onset of unilateral hip pain; if mild, may still bear weight; severe cases involve inability to walk, leg shortening, and external rotation | X-ray or MRI | Surgical repair or replacement; pain management, rehabilitation | High mortality rate in the elderly (12-37% within a year) |
| Pelvic Fracture | High-impact trauma (e.g., motor vehicle accident) | Symptoms vary depending on severity; may include bruising, swelling, incontinence, or numbness | X-ray, CT scan | Stabilization, pain management, surgery if severe | Can lead to internal bleeding, life-threatening injuries |
| Cauda Equina Syndrome | Spinal nerve compression | Acute onset of saddle anesthesia, bowel/bladder incontinence, bilateral leg numbness/weakness | MRI or CT scan | Emergency spinal decompression surgery | Requires immediate treatment to prevent permanent nerve damage |
| Medial Tibial Stress Syndrome (Shin Splints) | Overuse injury (common in runners) | Gradual onset of shin pain, worsens over time, tenderness along the tibia | X-ray often normal; bone scan or MRI for stress fractures | Rest, ice, compression, elevation (RICE); cushioned footwear; stretching | More common in runners and individuals with flat feet; linked to female athlete triad |
| Plantar Fasciitis | Microtears in plantar fascia | Heel pain that worsens with walking, especially in the morning or after prolonged standing | X-ray to rule out fractures or heel spurs | NSAIDs, orthotics, stretching exercises, podiatry referral | Increased risk in obesity, diabetes, prolonged standing |
| Morton’s Neuroma | Nerve irritation between 3rd and 4th metatarsals | Burning/numbness in forefoot, “pebble-like” sensation; worsens with high heels or tight shoes | Mulder test (MTP squeeze) – positive if clicking and pain occur | Avoid tight/high-heeled shoes, use forefoot padding, refer to podiatry | More common in runners, dancers, and individuals who wear tight shoes |
| Degenerative Joint Disease (Osteoarthritis) | Breakdown of cartilage over time | Gradual onset of joint pain, stiffness (morning stiffness <15 min), tenderness, swelling; Heberden’s (DIP) and Bouchard’s (PIP) nodes | X-ray: joint space narrowing, osteophytes, effusion; bone density test to rule out osteoporosis | Pain management (acetaminophen, NSAIDs, topical gels), physical therapy, weight loss, steroid injections if needed | Commonly affects weight-bearing joints (hips, knees, hands); risk increases with age and joint overuse |
| Hip Pain Location | Possible Causes |
|---|---|
| Outer hip pain, worsened by pressure | Trochanteric bursitis |
| Pain during movement, relieved by rest | Structural joint issue, osteoarthritis (OA) |
| Persistent pain, especially at night | Infection, inflammation, or neoplastic conditions |
| Pain in the front of the hip/groin | Hip joint involvement (e.g., osteoarthritis) |
| Pain in the back of the hip | Sacroiliac (SI) joint dysfunction, lower back pathology |
| Condition | Cause | Signs & Symptoms | Diagnostics | Treatment | Concerns |
|---|---|---|---|---|---|
| Systemic Lupus Erythematosus (SLE) | Autoimmune | Butterfly-shaped rash on face (malar rash), worsens with sun exposure; non-itchy, thick, scaly rashes on sun-exposed areas (discoid rash); fatigue, oral ulcers, gastritis; chronic inflammation affecting skin, joints, kidneys, lungs, nervous system, and serous membranes | ANA positive, ↑ ESR, anemia, proteinuria in urine analysis | Refer to rheumatology; topical & oral steroids, Plaquenil, methotrexate, biologics (DMARDs); sun protection (avoid exposure 10 AM–4 PM, use non-fluorescent bulbs) | Characterized by periods of remission & relapse; more common in women (20s-30s); mild cases may present as cutaneous lupus; increased risk of miscarriage |
| Rheumatoid Arthritis (RA) | Autoimmune; multiple joint inflammation & damage | Gradual onset; fatigue, low-grade fever, muscle aches, morning stiffness (>1 hour); swollen, warm, painful joints affecting fingers, hands, wrists, ankles, feet, shoulders; “sausage fingers,” swan neck deformities, Bouchard’s nodes | Symmetrical joint involvement for ≥6 weeks; ↑ ESR, mild microcytic/normocytic anemia, positive rheumatoid factor & anti-CCP; radiographs show joint space narrowing | Refer to rheumatology; NSAIDs, steroids, DMARDs, TNF inhibitors (Humira, Enbrel) | Can cause eye complications (uveitis, scleritis), pericarditis, increased malignancy risk; peak onset between ages 20-40 |
| Gout | Uric acid crystal buildup in joints (most commonly the great toe) | Sudden onset of painful, swollen, red joint (typically big toe – podagra); limping due to severe pain; triggered by alcohol, red meat, seafood; exacerbated by medications (aspirin, diuretics, cyclosporine, niacin) | Tophi deposits on ears/joints; elevated uric acid (test 2 weeks after an attack); ↑ ESR; Gold standard: joint aspiration | Pain relief is primary goal; NSAIDs (Indomethacin, Naproxen), colchicine; Avoid starting allopurinol during acute attacks, but do not discontinue if already prescribed; long-term treatment: allopurinol, probenecid | Can lead to joint damage; more common in men >30, obese individuals; Pseudogout (calcium pyrophosphate crystals) linked to parathyroid disease |
| Ankylosing Spondylitis | Chronic inflammatory disorder affecting the spine | Chronic back pain (>3 months), worsens at night, improves with movement; stiffness, fatigue, chest pain with breathing, reduced range of motion, possible buttock pain; associated with uveitis (eye pain, light sensitivity, redness) | ↑ ESR, CRP; RF negative; “bamboo spine” on X-ray | Refer to rheumatology; NSAIDs (can cause GI damage by inhibiting COX-1 & COX-2); if uveitis, refer to ophthalmology | Can cause anterior uveitis, aortitis, spine fusion (leading to limited motion), and spinal stenosis |
| Meniscus Tear (Knee) | Trauma or overuse (twisting injury) | Knee pain with locking, popping, or giving out; difficulty extending knee fully; limping; joint line tenderness | McMurray’s test, Apley’s grinding test, decreased ROM; X-ray (though meniscus doesn’t show); MRI | RICE therapy, joint effusion management; aspiration if no improvement in 2-4 weeks; crutches & knee immobilizer; straight leg raises to strengthen quadriceps; refer to orthopedics | |
| Bursitis (Ruptured Baker’s Cyst) | Fluid-filled bursa rupture behind knee | May be asymptomatic or present as a noticeable mass behind the knee; rupture can mimic cellulitis with redness, swelling, tenderness | Clinical diagnosis, MRI to rule out a septic joint | RICE, NSAIDs; large cysts may require drainage; if fluid appears cloudy, send for culture to rule out infection | |
| Sarcoidosis | Inflammatory disease causing non-caseating granulomas, mainly in lungs, lymph nodes, eyes, and skin | Gradual or rapid onset; fatigue, fever, weight loss, joint pain, rash, skin nodules, eye irritation (blurred vision, redness, photosensitivity) | Serum amyloid A, soluble interleukin-2 receptor, ACE, glycoprotein KL-6; hypercalcemia, hypercalciuria; chest X-ray, CT chest, PFT, biopsy | Often self-limiting; NSAIDs, corticosteroids (oral, topical, or inhaled), Plaquenil, DMARDs; lung transplant in severe cases | More common in adults 20-40, particularly women & African Americans |
| Reactive Arthritis (Reiter’s Syndrome) | Autoimmune response to infection (e.g., GI or genitourinary) | Develops after infection (diarrhea or STI); joint pain (knees, ankles, feet); dactylitis (sausage digits); heel pain, cervicitis, prostatitis, conjunctivitis, uveitis, urethritis, genital ulcers | HLA-B27 positive; joint cultures negative; symptoms may vary based on infection source | NSAIDs, systemic corticosteroids, TNF inhibitors (etanercept, infliximab); urethritis treated with doxycycline (7 days) or azithromycin (single dose) | Often follows bacterial infections (e.g., Shigella, Salmonella, Campylobacter, Chlamydia); affects both genders equally if GI-related, but urethritis cases are more common in males |