Sexually Transmitted Diseases
| Condition | Cause | Symptoms/Signs | Diagnosis | Treatment | Concerns |
|---|---|---|---|---|---|
| HIV | HIV-1 is the most prevalent in the U.S. | Hairy leukoplakia (from Epstein-Barr virus), recurrent thrush, fever, weight loss, diarrhea, cough, shortness of breath, Kaposi’s sarcoma; symptoms typically appear within 2-4 weeks | Initial screening is done with a 4th-generation HIV antigen/antibody combination test, which detects both HIV-1/2 antibodies and the p24 antigen (present earlier in infection). If positive, it is confirmed with an HIV-1/HIV-2 differentiation immunoassay. The Western blot is no longer used for confirmation. If results are indeterminate or discordant, an HIV RNA (PCR) test is performed to check for acute infection. A normal CD4 count ranges from 500 to 1500 cells/mm³. HIV antibodies typically become detectable within 3 to 12 weeks after exposure. | Treatment and Prevention: – Prophylaxis: Begin daily Bactrim (TMP-SMX) when CD4 count falls below 200 to prevent Pneumocystis jirovecii pneumonia. Alternatives for sulfa-allergic patients include dapsone, atovaquone, or aerosolized pentamidine. – Toxoplasma gondii prophylaxis is indicated when CD4 <100, often using Bactrim as well. Patients should avoid exposure to cat litter, undercooked pork, bird droppings, and gardening without gloves. – Pregnancy: HIV-positive pregnant women should begin zidovudine (AZT) as early as possible. Newborns should receive prophylaxis within 6–12 hours of birth. – Antiretroviral therapy (ART): Monitoring includes watching for nephrotoxicity with tenofovir and bone marrow suppression with zidovudine. – Treatment success is best indicated by a decrease in viral load, not CD4 count alone. PrEP and PEP: – PrEP (Pre-exposure prophylaxis): Daily tenofovir-emtricitabine (e.g., Truvada or Descovy) is the standard and reduces HIV transmission risk by ~99% when taken consistently. – PEP (Post-exposure prophylaxis): Should be initiated immediately after exposure, ideally within 2 hours (and no later than 72 hours), and continued for 28 days. – Injectable long-acting PrEP is available but may exceed board exam scope. | – AIDS is defined by a CD4 count <200 cells/mm³ or the presence of an AIDS-defining illness. – Pneumocystis jirovecii pneumonia remains a leading cause of death among HIV patients if prophylaxis is not maintained. |
| Disseminated Gonococcal Disease | N. gonorrhoeae infection | Petechial or pustular skin lesions on hands/soles; tender, swollen joints, particularly in one large joint like the knee. May show signs of an STD or pharyngitis with green, purulent discharge | NAAT testing for pharynx/rectal sites; GenProbe for cervix/urethra | Ceftriaxone 1-gram IM or IV every 24 hours | Persistent symptoms or complications may arise if untreated. |
| Chlamydia trachomatis | Atypical bacteria, incubation of 7-14 days | Often asymptomatic; can occur in cervix, urethra, fallopian tubes, endometrium. Can lead to pelvic inflammatory disease (PID), presenting with fever, abdominal pain, and abnormal discharge | NAAT testing for various sites; GenProbe for cervix/urethra | Azithromycin 1g, Doxycycline 100mg x7 days; treatment for sexual partners is also required. Test for cure in pregnant women 3 weeks post-treatment. | Risk of PID especially in those under 25. Chandelier’s sign is indicative of PID. |
| Neisseria gonorrhoeae | Gram-negative diplococci bacteria | Purulent green discharge from the penis or vagina; may cause cervicitis, urethritis, pharyngitis, rectal infection. Many cases are asymptomatic, especially in females | NAAT (nucleic acid amplification test) for pharyngeal and rectal sites; GenProbe or NAAT for cervical or urethral specimens | Ceftriaxone 500 mg IM once (for <150 kg; use 1 g if ≥150 kg) + Doxycycline 100 mg PO BID x 7 days if chlamydial coinfection has not been ruled out Avoid routine azithromycin due to resistance concerns | Often co-occurs with Chlamydia trachomatis—assess and treat empirically if coinfection possible. Gonorrhea may infect multiple anatomical sites (genital, rectal, pharyngeal). Treatment must address all exposed sites. |
| Syphilis | Treponema pallidum (spirochete bacterium), with an incubation period of 2–4 weeks. | – Primary stage: Painless chancre (ulcer) at the site of infection, along with swollen lymph nodes. – Secondary stage: Non-itchy rash on palms/soles, mucosal lesions, fever, sore throat, weight loss. – Tertiary stage: Organ damage, neurosyphilis (can affect the nervous system). | – RPR or VDRL for initial screening. – Confirm with FTA-ABS or treponemal antibody tests (as part of the “reverse sequence” algorithm). – A positive non-treponemal test (like RPR/VDRL) is confirmed by a specific treponemal test. | – Benzathine penicillin G 2.4 million units via IM injection (single dose). – If allergic to penicillin, doxycycline can be used as an alternative. – For latent syphilis, repeat doses for 3 weeks. | – Syphilis is most contagious during the secondary stage. – False positives can occur in cases of pregnancy, Lyme disease, or autoimmune diseases. – Be aware of the Jarisch-Herxheimer reaction after treatment, which is a temporary worsening of symptoms, often seen within 24 hours. |
| Fitz-Hugh-Curtis Syndrome (Perihepatitis) | Gonococcal or chlamydial infection leading to liver capsule scarring | Complaints of right upper quadrant (RUQ) pain, often linked to PID | Liver function tests typically normal | Treat as complicated gonococcal or chlamydial infection with Rocephin + doxycycline, possibly adding Flagyl | Can cause liver scarring, requires extended treatment. |
| Condition | Cause | Signs/Symptoms | Diagnosis | Treatment | Considerations |
|---|---|---|---|---|---|
| Reiter’s Syndrome | Immune response triggered by bacterial infection (usually Chlamydia) | Most common in men. Characterized by a history of chlamydia with red, swollen, migrating joints (migratory arthritis). Commonly referred to as “can’t see, pee, or climb a tree” due to symptoms of conjunctivitis, urethritis, and arthritis. | Clinical assessment based on symptoms | Symptom relief with NSAIDs | Typically resolves without complications. Recurrence can be reduced with early treatment. |
| Genital Warts (Condyloma Acuminata) | HPV, particularly types 16 and 18, is strongly associated with cervical, anal, oropharyngeal, and other cancers. | Lesions caused by HPV are typically soft, flesh-colored, and may be pedunculated, flat, or papular. When acetic acid is applied during examination, lesions may appear white. | Pap smear and colposcopy | Topical therapies for genital warts include imiquimod (Aldara) cream and podofilox (Condylox) solution or gel, which are applied directly to lesions. Procedural options such as cryotherapy (freezing) are also commonly used, especially for external warts. During pregnancy, only chemical cauterizing agents such as bichloracetic acid or trichloroacetic acid are considered safe and appropriate for use; other treatments are contraindicated due to potential fetal risk. | Vaccination against HPV is a key preventive measure. The Gardasil 9 vaccine is: – Routinely recommended for all boys and girls aged 11–12 (can begin as early as age 9) to reduce the risk of genital warts and HPV-related cancers. – Catch-up vaccination is advised for anyone through age 26 who did not receive the full series. – For adults aged 27 to 45, vaccination may be considered based on shared clinical decision-making, particularly for those at ongoing risk for new HPV exposure (e.g., new or multiple sexual partners). |
| Herpes Simplex Virus (HSV-1 & HSV-2) | HSV-1 affects oral mucosa; HSV-2 affects genital area | Initial signs include itching, burning, and tingling at the infection site, followed by the appearance of painful blisters on a red base. These can rupture and cause discomfort. Outbreaks last 2-4 weeks. The virus can spread even when there are no visible symptoms. | Herpes culture or RPR assay; Tzanck smear (though outdated) | Antiviral treatments such as Acyclovir (Zovirax), Famciclovir (Famvir), and Valacyclovir (Valtrex) reduce symptoms. Episodic therapy can alleviate symptoms, while suppressive treatment reduces recurrence. | HSV can be transmitted even without symptoms, shedding 10% of the time. |
| Chancroid | Haemophilus ducreyi (Gram-negative bacterium) | Painful, soft ulcers with a necrotic base appear at the site of inoculation. Multiple lesions are common. | Culture for Haemophilus ducreyi (sensitivity <80%) | Azithromycin, ciprofloxacin, or ceftriaxone for treatment. Encourage safe sex practices, STI testing, and hepatitis vaccination. | Prevention includes condom use, limiting sexual partners, and regular STI screenings. |
| Lymphogranuloma Venereum | Chlamydia trachomatis (serovars L1, L2, L3) | Symptoms develop 1-4 weeks after exposure, starting with a vesicular or ulcerative lesion, progressing to painful inguinal lymph nodes (buboes) that may drain. | PCR test for Chlamydia trachomatis | Doxycycline or erythromycin are used for treatment. Lifestyle changes to limit sexual partners and regular STI screenings are recommended. | Timely treatment is necessary to avoid complications like lymph node enlargement and chronic symptoms. |
| Pelvic Inflammatory Disease (PID) | N. gonorrhoeae, C. trachomatis, Bacteroides, Enterobacteriaceae, and streptococci | Symptoms include abdominal pain, fever, cervical motion tenderness, and abnormal vaginal discharge. | Diagnosis is primarily clinical, supported by testing for gonorrhea and chlamydia. | For outpatient treatment of Pelvic Inflammatory Disease (PID), the current CDC recommendation is a single intramuscular dose of ceftriaxone 500 mg (or 1 g if the patient weighs ≥150 kg), combined with doxycycline 100 mg taken orally twice daily for 14 days, and metronidazole 500 mg taken orally twice daily for 14 days. This combination provides coverage for Neisseria gonorrhoeae, Chlamydia trachomatis, and anaerobic organisms. The addition of metronidazole is important for treating potential anaerobic infections associated with PID. | PID increases the risk of ectopic pregnancy and infertility. Early treatment is crucial to prevent long-term complications. |
| Trichomoniasis | Trichomonas vaginalis, a protozoan parasite with flagella | Symptoms include dysuria, itching, vulvovaginal irritation, and a yellow-green frothy discharge. A “strawberry cervix” with some bleeding is often seen. | Wet mount smear showing motile protozoa and high white blood cell count | Metronidazole (Flagyl) 2g orally, tinidazole (2g orally), or metronidazole (500mg twice daily for 7 days). Avoid alcohol during treatment. Treat sexual partners. | Routine screening is recommended for sexually active individuals under 25. Pregnant women and men who have sex with men should also be screened regularly. |
Annual Screening Recommendations:
- For sexually active individuals under 25: Test for Chlamydia and gonorrhea
- HIV: Annual tests for syphilis, chlamydia, and gonorrhea
- Men who have sex with men: Yearly tests for chlamydia, gonorrhea (including pharyngeal), HIV, syphilis, and HBsAg
- Pregnant women: Screen for HIV, chlamydia, gonorrhea, syphilis, and HBsAg during the first prenatal visit
Men’s Health
Prostate Organ
| Condition | Physical Examination Findings | Comparison to Touch Sensation |
|---|---|---|
| Normal Prostate | Firm, smooth, and non-tender | Feels similar to pressing on the tip of your nose |
| Acute Prostatitis | Tender, swollen (boggy), and firm with induration | Feels similar to pressing on your cheekbone |
| Benign Prostatic Hyperplasia (BPH) | Firm, smooth, symmetrically enlarged | Feels similar to pressing on the tip of your nose |
| Prostate Cancer | Asymmetrical, nodular, hard, and non-tender | Malignant lesions are typically not detectable until advanced stages; PSA production may be elevated |
Interesting facts:
- Sperm are generated in the seminiferous tubules within the testes.
- It takes approximately three months for sperm to fully mature, during which they are stored in the epididymis.
- The production of testosterone is triggered by the release of luteinizing hormone.
- Testosterone and follicle-stimulating hormone play key roles in stimulating spermatogenesis.
- Transillumination is useful for assessing testicular swelling, masses, bleeding, or undescended testes:
- Hydroceles will transilluminate.
- Tumors and varicoceles (which resemble a “bag of worms”) do not transilluminate.
- Postrenal azotemia may result from prolonged urinary obstruction, potentially leading to hydronephrosis and kidney dysfunction.
- If scrotal swelling is present without pain, evaluate for systemic weakness and consider referring to a urologist.
| Condition | Cause | Signs & Symptoms | Diagnostics | Treatment | Concerns |
|---|---|---|---|---|---|
| Priapism | Sickle cell disease, ED medications, cocaine use, quadriplegia | Persistent, painful erection lasting several hours | — | Medical emergency requiring urgent intervention | May lead to permanent erectile dysfunction if untreated |
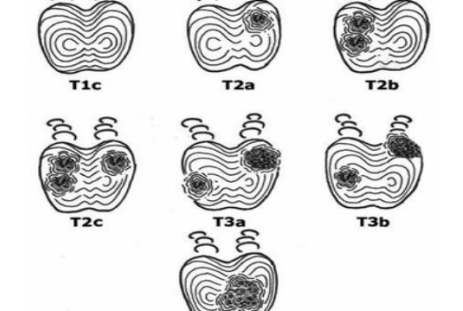
| Testicular Cancer | — | Adolescent or young adult presenting with a painless nodule, heaviness, or noticeable enlargement of one testicle; may feel a hard, fixed nodule; often asymptomatic until metastasis | Ultrasound for solid mass, Gold standard: testicular biopsy | Immediate referral to urology for biopsy and treatment | Higher incidence in white males (ages 15-35), rare in African Americans; Cryptorchidism increases cancer risk |
| Prostate Cancer | Second most common cancer in men | Prostate cancer may present with a hard, fixed nodule and asymmetrical prostate enlargement on exam, most commonly in older males. Some individuals may experience erectile dysfunction, lower back pain, weak urine stream, or nocturia, though many remain asymptomatic in early stages. | Screening typically involves a digital rectal exam (DRE) and prostate-specific antigen (PSA) testing. PSA > 4.0 ng/mL may warrant further evaluation, although >2.5 ng/mL is considered significant in high-risk individuals. Prostate biopsy is used to confirm diagnosis. Current Screening Guidelines (USPSTF): Ages 55–69: PSA screening is not routinely recommended; instead, it should involve shared decision-making based on individual risk factors, family history, and personal values. Ages ≥70: Routine PSA screening is not recommended. | Patients with elevated PSA levels or suspicious findings should be referred to urology. Treatment may include antiandrogens (e.g., Finasteride) and hormone blockers (e.g., Leuprolide [Lupron]). | Increased risk is seen in African American men, Jamaican men, and individuals with obesity. Finasteride is teratogenic; women who are pregnant or may become pregnant should avoid handling crushed or broken tablets. |
| Torsion of Appendix Testis (Blue Dot Sign) | Infarction/necrosis of appendix testis (not testicular torsion) | School-aged child with sudden onset of a small, blue-colored mass on the testicular surface (“blue dot sign”) | — | Emergency referral to the ER | Appendix testis is a small polyp-like structure attached to the testicle |
| Hernia | — | — | Inguinal hernia identified on physical exam | Surgical repair | — |
| Benign Prostatic Hyperplasia (BPH) | Non-cancerous prostate enlargement | Lower urinary tract symptoms (LUTS): nocturia, difficulty initiating urination, weak stream, dribbling, incomplete bladder emptying, urinary retention | Rectal exam: firm, smooth, symmetrically enlarged prostate; PSA levels should be doubled when on Flomax or Proscar | Lifestyle changes: reduce caffeine/alcohol, limit fluids before bed; medications include alpha-blockers (Terazosin, Tamsulosin), 5-alpha reductase inhibitors (Finasteride); refer to urology if severe | Common in 50% of men over 50 and 80% over 70; avoid antihistamines, decongestants, caffeine, amitriptyline; saw palmetto may provide symptom relief |
| Chronic Bacterial Prostatitis | Persistent prostate infection (>6 weeks), often due to E. coli or Proteus | History of recurrent UTIs or asymptomatic; may present with prolonged suprapubic or perineal discomfort, irritative voiding symptoms (dysuria, nocturia, frequency) | Prostate exam typically normal; UA and culture for diagnosis | First-line: Trimethoprim-sulfamethoxazole (Bactrim); alternatives: ofloxacin or levofloxacin (if sensitive); treat for 4-6 weeks | Requires long-term antibiotic therapy to prevent recurrence |
| Acute Prostatitis | Bacterial infection (E. coli, Proteus, or STI pathogens) | Sudden onset of high fever, chills, suprapubic or perineal pain, dysuria, frequency, nocturia, cloudy urine; may radiate to back/rectum; severe discomfort when sitting or during bowel movements | Rectal exam: prostate is enlarged, boggy, warm, and tender; CBC, UA, and culture | <35 years: Ceftriaxone + doxycycline (STI-related) >35 years: Ciprofloxacin or Levaquin for 6 weeks; also NSAIDs, sitz baths, hydration, stool softeners | Avoid vigorous prostate palpation to prevent septicemia |
| Condition | Cause | Signs & Symptoms | Diagnostics | Treatment | Concerns |
|---|---|---|---|---|---|
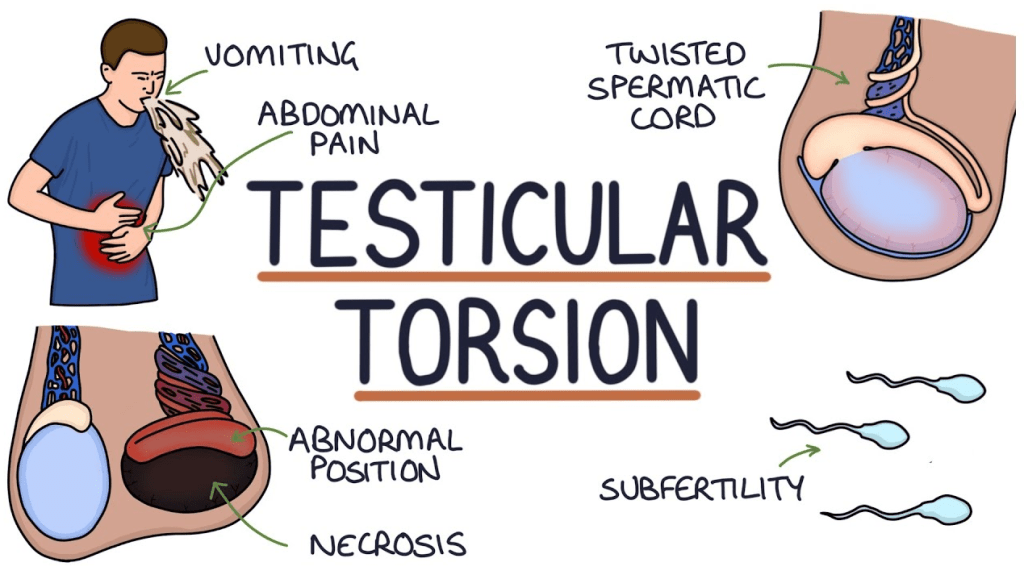
| Testicular Torsion | Twisting of the spermatic cord, cutting off blood flow to the testicle | Sudden, severe scrotal pain with swelling and redness; nausea/vomiting common; affected testicle sits higher and closer to the body (more often on the left side) | Absent cremasteric reflex (testicle fails to rise with inner thigh stimulation), UA, ultrasound (performed in the ER) | Urologic emergency – surgery within 6 hours to save the testicle (>85% survival rate); orchiopexy performed to prevent recurrence | Most common in ages 10-20, increased risk with bell clapper deformity |
| Epididymitis | Inflammation (infectious or non-infectious) | Gradual onset of painful, swollen, red scrotum; unilateral testicular tenderness, possible discharge; swelling and induration of the posterior epididymis; often linked to prolonged sitting | CBC, UA, culture; + Prehn’s sign (pain relief with scrotal elevation), + Cremasteric reflex; STI testing if suspected | <35 years: Doxycycline (10 days) >35 years: Ofloxacin or levofloxacin (10 days); NSAIDs, scrotal elevation/support | Scarring of the vas deferens can lead to infertility |
| Erectile Dysfunction (ED) | Vascular insufficiency (diabetes, hypertension), neuropathy, medications (SSRIs, beta-blockers), smoking, alcohol use, hypogonadism | Inability to maintain an erection firm enough for intercourse | — | Phosphodiesterase-5 inhibitors (PDE5Is): Viagra (take on empty stomach), Levitra (take before intercourse), Cialis (effective up to 36 hours) | Side effects: headache, flushing, dizziness, hypotension, nasal congestion, priapism; Contraindicated with nitrates, caution with alpha-blockers, post-MI or stroke |
| Peyronie’s Disease | Inflammation leading to fibrous plaque formation in the penis | Penile pain (mainly during erection), palpable nodules (fibrotic plaques), curved or bent erection | — | Refer to urology | Condition may improve, remain stable, or worsen over time |
| Balanitis | Candida infection | Inflammation of the glans penis, more common in uncircumcised men, diabetics, and immunocompromised individuals | — | OTC antifungal creams (azole-based); treat sexual partner | Recurrent infections may indicate undiagnosed diabetes |
| Phimosis | Foreskin tightness due to edema or scarring | Inability to retract the foreskin over the glans penis; typically seen in neonates | — | — | May require circumcision if persistent or causing urinary issues |
| Varicocele | Dilated veins within the scrotum | “Bag of worms” appearance, present only when standing; may cause recurrent scrotal pain; new-onset varicocele can indicate a tumor obstructing venous drainage | Scrotal ultrasound | Treatment if causing pain, testicular atrophy, or infertility: surgical repair or percutaneous embolization; scrotal support for mild cases | Can reduce sperm count, affecting fertility |
| Hydrocele | Fluid accumulation around the testicle, often associated with a hernia | Painless scrotal swelling that transilluminates (glows when light is passed through) | Scrotal ultrasound | Refer to urology if needed | Non-communicating type usually resolves within the first year of life, leaving the scrotum appearing deflated afterward |