Women’s Health
Miscellaneous Genitourinary (GU) Facts
Characteristics of a Healthy Reproductive-Age Woman:
- Vaginal Discharge: Typically white, clear, and flocculent, with a daily volume of ½ to 1 teaspoon.
- Normal Vaginal pH: Ranges between 3.8 and 4.2.
Additional Testing for STIs:
- If any STI is detected, screening for syphilis, HIV, and hepatitis B is also recommended.
Friable Cervix:
- Bleeds easily when touched with a cotton swab.
- Higher susceptibility to STI acquisition.
Expected Pelvic Exam Findings in Postmenopausal Women:
- Vaginal rugae appear flattened.
- Minimal white vaginal discharge is normal.
- Ovaries should not be palpable.
Loss of Bladder Control
| Type | Description | Management Strategies | Common Age Group |
|---|---|---|---|
| Stress Incontinence | Leakage triggered by activities such as laughing, sneezing, bending, or lifting. | Pelvic floor strengthening exercises (Kegels), possible use of decongestants. | Most common between ages 45-49. |
| Overflow Incontinence | Continuous dribbling or weak urine stream due to bladder outlet obstruction. | Address underlying cause (e.g., benign prostatic hyperplasia (BPH), multiple sclerosis, spinal cord injury). | More frequent in older men. |
| Urge Incontinence | Sudden, intense urge to urinate due to overactive bladder and detrusor muscle instability. | Antimuscarinic medications (e.g., oxybutynin/Ditropan), tricyclic antidepressants (e.g., imipramine), Kegel exercises. | More common in older women. |
| Functional Incontinence | Inability to reach the toilet in time due to mobility issues or physical limitations. | Use of bedside commodes, raised toilet seats with handles, physical therapy for mobility and strength improvement. | Varies based on mobility impairment. |
| Mixed Incontinence | Combination of both stress and urge incontinence symptoms. | Pelvic floor exercises (Kegels) for strengthening bladder control. | Occurs in various age groups. |
Reversible Causes of Bladder Leakage:
D – Delirium
I – Infections (e.g., urinary tract infection)
A – Atrophic urethritis & vaginitis
P – Pharmaceuticals (e.g., diuretics, certain medications)
E – Excessive urine production (linked to heart failure, poorly controlled or undiagnosed diabetes)
R – Restricted mobility
S – Severe stool impaction
Contributing Factors:
- Obesity
- Pregnancy
- Vaginal childbirth
- Menopause
- Aging
- Diabetes
Foods & Beverages That May Worsen Symptoms:
- Caffeinated drinks (tea, coffee, soda)
- Alcohol
- Carbonated beverages
- Citrus fruits
- Spicy foods
Bladder and Pelvic Organ Prolapse
- Gynecological Exam: Have the patient cough to increase intra-abdominal pressure, making herniation more noticeable.
- Bladder Herniation (Cystocele):
- Anterior vaginal wall bulge
- May require pessary placement or surgical intervention
- Rectal Herniation (Rectocele):
- Posterior vaginal wall bulge
- Symptoms: Rectal fullness, possible fecal leakage
- Management: Kegel exercises, avoiding straining during bowel movements, treating constipation
- May need pessary or surgery
- Uterine Prolapse:
- Cervix moves downward into the vaginal canal
- Symptoms: Sensation of vaginal heaviness, low back discomfort
- Avoid heavy lifting; may require pessary or surgical correction
- Enterocele:
- Small intestine shifts into the space between the uterus and posterior vaginal wall
- Symptoms: Pelvic pressure, pulling sensation, lower back pain, painful intercourse (dyspareunia)
Breast Cancer Overview
- BRCA Genes: Genetic mutations linked to increased breast cancer risk.
- High-Risk Factors:
- Family history of breast cancer diagnosed before age 50.
- Triple-negative breast cancer diagnosed before age 60.
- History of ovarian or other gynecological cancers.
- Fewer pregnancies (low parity), early onset of menstruation (menarche), and late menopause.
- BRCA in Men:
- Increased risk for both breast and prostate cancer.
- Referral and Screening:
- High-risk individuals should see a breast specialist.
- Screening includes MRI and mammograms.
- Begin screening 10 years before the earliest family diagnosis.
- Genetic Prevalence:
- More frequently found in Ashkenazi Jewish populations.
Uterine Fibroids (Leiomyoma/Myoma)
- Fibroid Growth & Symptoms:
- Noncancerous tumors that can cause uterine enlargement.
- Common symptoms: Heavy menstrual bleeding (menorrhagia), pelvic discomfort or cramping, and spotting between cycles.
- Potential Risks:
- Typically benign, but in rare cases, can develop into uterine cancer (leiomyosarcoma).
Phases of the Menstrual Cycle
- Follicular Phase (Days 1–14):
- Estrogen is the dominant hormone, promoting endometrial growth and thickening.
- Follicle-Stimulating Hormone (FSH) from the anterior pituitary stimulates follicle maturation, leading to estrogen production.
- Ovulatory Phase (Mid-Cycle, Day 14):
- Luteinizing Hormone (LH) surge from the anterior pituitary triggers ovulation.
- Luteal Phase (Days 14–28):
- Progesterone becomes the dominant hormone, preparing the uterus for potential implantation.
- Fertility Window:
- Greatest likelihood of conception occurs when intercourse happens 1–2 days before ovulation.
Common Diagnostic Tests
- Tzanck Smear: Identifies herpes infections, revealing large multinucleated cells.
- Gram Stain: Used to detect Neisseria gonorrhoeae, though rarely utilized.
- Whiff Test: Assesses for bacterial vaginosis (BV).
- KOH Preparation: Helps diagnose fungal infections by breaking down skin cells to expose fungal elements.
Cervical Changes
- Cervical Ectropion:
- Appears as bright red, irregular, bumpy tissue around the cervical os.
- Benign but more prone to bleeding (friable).
- Frequently seen in women using birth control.
- May alter in size, shape, or even regress over time.
- Pap Smear Consideration:
- Always sample the transformation zone (squamocolumnar junction).
- The junction between the bright red ectropion and the smoother cervical surface is the most likely site for abnormal cell development.

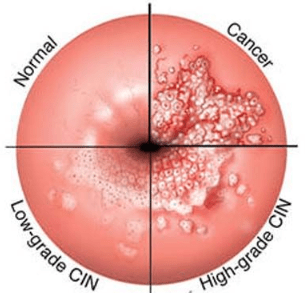
Cervical Cancer Screening:
Begin screening at age 21 with a Pap smear every 3 years through age 29.
From ages 30 to 65, patients have three acceptable options:
- Pap + HPV co-testing every 5 years
- Pap smear alone every 3 years
- Primary high-risk HPV (hrHPV) testing alone every 5 years (per 2018 guidelines)
Screening may be discontinued after age 65 if there is adequate prior negative screening history, generally defined as:
- Three consecutive negative Pap tests or two negative co-tests in the past 10 years, with the most recent test within the past 5 years, and
- No history of CIN2+ (precancerous lesions) in the last 20 years
Women who have had a total hysterectomy (including removal of the cervix) for benign reasons do not require further screening.
A satisfactory Pap specimen should include both squamous epithelial and endocervical cells.
Abnormal Pap Results & Follow-Up:
Atypical Squamous Cells of Undetermined Significance (ASC-US):
- <20 years: Repeat in 1 year
- 21–24 years: Repeat Pap in 1 year
- 25–29 years: Perform reflex HPV testing
- If HPV-positive → Repeat Pap in 1 year
- 30+ years:
- If HPV-positive → Refer for colposcopy
- If HPV-negative → Repeat co-testing in 3 years
Atypical Glandular Cells (Endometrial Cells):
- May suggest premalignancy or malignancy → Requires endometrial biopsy
Low-Grade Squamous Intraepithelial Lesions (LSIL):
- 21–24 years: Repeat Pap in 1 year
- 25–29 years: Colposcopy with cervical biopsy
- 30+ years:
- HPV-positive → Colposcopy with biopsy
- HPV-negative → Repeat in 12 months or proceed to colposcopy
High-Grade Squamous Intraepithelial Lesions (HSIL):
- 21–24 years: Colposcopy with cervical biopsy
- 25+ years: Immediate excisional treatment (e.g., LEEP or cervical conization)
HPV & Prevention:
- HPV types 16 and 18 are responsible for approximately 70% of cervical cancer cases
- Gardasil vaccine is recommended for prevention of HPV-related cervical disease
Miscellaneous Clinical Insights
- Puberty & Development:
- Breast asymmetry is normal in both boys and girls during puberty.
- Gynecomastia can occur in adolescent males and usually resolves on its own.
- Postmenopausal Ovarian Assessment:
- If an ovary remains palpable after menopause, conduct a transvaginal ultrasound to assess and rule out ovarian cancer.
- Primary Amenorrhea:
- Defined as the absence of menstruation by age 15, despite the presence of secondary sexual characteristics.
- Requires OB/GYN referral for evaluation of potential causes, including pituitary or hypothalamic disorders.
Oral Contraceptives Overview
Combined Oral Contraceptives (COCs)
- Monophasic Pills (e.g., Loestrin FE) – 21 active pills with 7 placebo (iron) tablets.
- Biphasic Pills (e.g., Ortho-Novum) – Two different progesterone doses throughout the cycle.
- Triphasic Pills (e.g., Ortho Tri-Cyclen) – 21 active pills with 7 placebo tablets; hormone levels vary weekly. Beneficial for acne management.
- Extended Cycle Pills (e.g., Seasonale) – 84 days of active pills followed by 7 placebo days, resulting in only four periods per year. Breakthrough bleeding is common.
- Ethinyl Estradiol/Drospirenone (Yaz) – Contains drospirenone, beneficial for acne, PCOS, hirsutism, and PMDD. Higher risk for DVT and hyperkalemia. Monitor potassium if patient is taking ACEIs, ARBs, or K+-sparing diuretics due to increased risk of blood clots, stroke, and CAD.
- Low-Dose Pills – Contain 20-25 mcg of ethinyl estradiol.
Progestin-Only Pills (Minipill)
- Suitable for breastfeeding mothers.
- Must be taken at the same time daily to maintain effectiveness.
- If taken more than 3 hours late, use backup contraception (e.g., condoms).
- Micronor – 28 days of progestin-only pills. Initiate on day 1 of the menstrual cycle.
Starting a New Prescription
- Can be initiated after ruling out pregnancy.
- “Quick Start” – Begin immediately upon prescription.
- “Sunday Start” – First pill taken on the Sunday after menstruation begins, helps avoid weekend periods.
- “Day One Start” – First pill taken on the first day of the cycle, offering optimal protection.
- Follow-up in 2-3 months to monitor blood pressure and side effects.
Long-Term Benefits (After 5+ Years of Use)
- Reduced risk of ovarian and endometrial cancer.
- Decreased menstrual cramps and dysmenorrhea (due to lower prostaglandins).
- Alleviates endometriosis symptoms.
- Improves acne and reduces hirsutism (by lowering androgens).
- Prevents ovarian cyst formation (by suppressing ovulation).
- Regulates heavy/irregular periods, thereby reducing iron deficiency anemia (IDA).
Contraindications for Oral Contraceptives
Absolute Contraindications (Mnemonic: “My CUPLETS”)
- Migraines with focal neurological aura or age 35+ with migraines (even without aura)
- Coronary artery disease (CAD) or cerebrovascular accident (CVA) history
- Unexplained genital bleeding
- Pregnancy
- Liver disease or liver tumors
- Estrogen-dependent malignancies
- Thrombotic disorders (e.g., Factor V Leiden mutation, DVT, PE)
- Smokers aged 35 or older
Relative Contraindications
- Migraines in individuals over 35
- Smokers under 35
- Recent fractures or lower limb immobilization (e.g., cast)
- Hypertension
Issues with Oral Contraceptives
- Unexpected bleeding or spotting
- Menstrual cramps
- Medications: Mefenamic acid (Ponstel), Aleve, Advil, Anaprox
- Menorrhagia (heavy menstrual bleeding)
- Missed Pills
- 1 missed pill → Take two pills immediately and continue as usual
- 2 missed pills → Take two pills daily for two consecutive days and complete the pack (use backup contraception for the rest of the cycle)
- Medication Interactions
- May be less effective with anticonvulsants, antifungals, St. John’s wort, penicillins, tetracyclines, rifampin
- Signs of Thromboembolism (ACHES mnemonic)
- Abdominal pain
- Chest pain
- Headaches
- Eye disturbances (vision changes)
- Severe leg pain
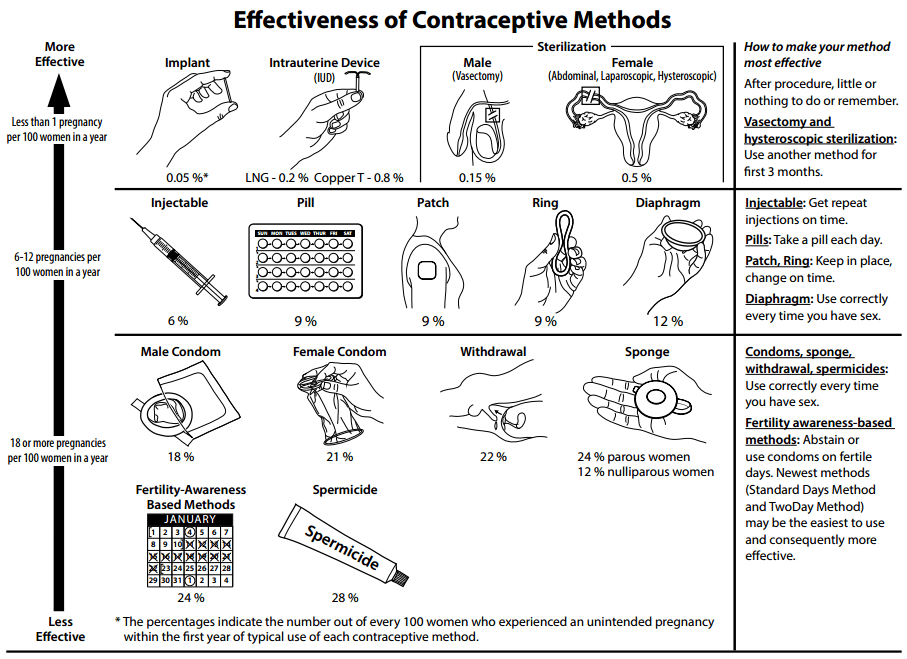
Alternative Contraceptive Methods
- Intrauterine Devices (IUDs) – Potential risks include infection, uterine perforation, and heavy menstrual bleeding
- ParaGard (Copper IUD):
- Non-hormonal
- Effective for up to 10 years
- May increase menstrual bleeding or cramping
- Mirena (Levonorgestrel IUD):
- Hormonal IUD
- Effective for up to 8 years (FDA-approved)
- Tends to reduce menstrual bleeding and cramping
- Slightly more effective than copper IUDs
- Skyla (Levonorgestrel IUD):
- Smaller than Mirena; designed for women who haven’t had children
- Effective for up to 3 years
- Releases a lower dose of hormone
- ParaGard (Copper IUD):
- Depo-Provera (Injectable Contraceptive) – 6% failure rate
- Administered every 3 months (within the first 5 days of cycle)
- Calcium + Vitamin D supplementation and weight-bearing exercise recommended
- Limit use to 2 years due to osteopenia/osteoporosis risk
- Not suitable for those with eating disorders (e.g., anorexia, bulimia)
- May delay fertility return – not ideal if pregnancy is planned within 12 months
- No interaction with Dilantin
- Barrier Methods
- Diaphragm with spermicide – 13% failure rate
- Must fully cover the cervix
- Keep in place for 6-8 hours after intercourse
- Apply fresh spermicide with each sexual act
- Cervical Cap – Can remain in for up to 72 hours (higher risk of UTIs and toxic shock syndrome)
- Condoms – 18% failure rate
- Diaphragm with spermicide – 13% failure rate
- Hormonal Contraceptives
- NuvaRing – 9% failure rate, worn for 3 weeks before removal
- Contraceptive Patch – 9% failure rate, increased risk of venous thromboembolism (VTE)
- Implants – <1% failure rate
- May take up to a year to resume ovulation after removal
- Possible weight gain
- Norplant lasts 5 years, Nexplanon lasts 3 years
Emergency Contraception
- Rule out pregnancy before administration
- Effective for up to 72 hours post-unprotected intercourse, with highest efficacy within 24 hours
- Works by inhibiting ovulation and slowing sperm and egg transport
Types of Emergency Contraception:
- Plan B – Progestin-only (89% effectiveness)
- Take first dose immediately, followed by second dose 12 hours later
- If vomiting occurs within 1 hour of ingestion, repeat the dose
- Ulipristal (Ella) – Prevents embryo implantation
- Approved for use up to 5 days after intercourse
- Follow-up – Seek medical attention if no menstrual period within 3 weeks
Condoms: Essential for STI Prevention
Consistent condom use significantly lowers the risk of sexually transmitted infections.
Alternative Contraceptive Methods
- Lactational Amenorrhea Method (LAM): A temporary but highly effective birth control method during exclusive breastfeeding.
- Emergency Contraception: Options such as emergency contraceptive pills or a copper IUD can greatly reduce the likelihood of pregnancy when used after unprotected intercourse.
| Condition | Cause | Signs & Symptoms | Diagnostics | Treatment | Concerns |
|---|---|---|---|---|---|
| Breast Mass/Cancer | – | Hard, irregular, painless lump, usually immobile and attached to skin/tissue. Most commonly found in the upper outer quadrant (Tail of Spence). Skin changes: dimpling, retraction, peau d’orange, bloody discharge, nipple changes. | According to the latest USPSTF draft guidance, routine mammography should begin at age 40 and be conducted every two years for women aged 40–74. This update reflects recent evidence supporting earlier detection. The American Cancer Society (ACS) continues to recommend that women have the option to begin annual screening at age 40, with a strong recommendation to start yearly screening by age 45. For women under 30, ultrasound is typically used as the initial imaging modality. Breast biopsy may be performed if further evaluation is needed. | Surgical referral. | BRCA screening (e.g., FHS-7 questionnaire). If BRCA-positive, consider genetic counseling. |
| Paget’s Disease of the Breast | – | Chronic scaly, red rash resembling eczema on the nipple, which does not heal. Itching, crusting, ulceration, and/or bleeding. Gradual enlargement. | – | – | May indicate ductal carcinoma in situ (DCIS). |
| Inflammatory Breast Cancer | – | Rapid-onset swelling, warmth, and redness in the breast, often in younger women. Mimics mastitis but lacks a distinct lump. Skin may appear bruised or pitted. | – | – | Aggressive breast cancer, more common in African American women. |
| Ovarian Cancer | 5th most common cancer in women | Nonspecific symptoms: bloating, pelvic or abdominal discomfort, low-back pain, urinary frequency, and constipation. Often diagnosed at an advanced stage due to vague presentation. | BRCA1/BRCA2 genetic screening starting at age 30. | – | Risk factors: Family history, BRCA mutation, endometriosis, obesity, early menstruation, late menopause, infertility. |
| Ectopic Pregnancy | Implantation outside the uterus | Symptoms appear 6-8 weeks after last menstrual period. Sexually active woman with light bleeding, one-sided lower abdominal/pelvic pain that worsens when supine or with movement. May refer to the right shoulder. | Serial quantitative hCG (should double every 24-72 hours but does not in ectopic pregnancy). | – | Leading cause of first-trimester maternal mortality. |
| Fibrocystic Breast Disease | – | Breast tenderness and palpable lumps appearing up to two weeks before menstruation, resolving afterward. No skin changes, nipple discharge, or lymph node involvement. | – | Avoid caffeine. Vitamin E and evening primrose oil supplementation. Supportive bras. | Benign, but symptoms can be bothersome. |
| Polycystic Ovarian Syndrome (PCOS) | Hormonal imbalance, insulin resistance, excess androgens | Presents in adolescence or early adulthood. Symptoms include irregular periods (oligomenorrhea/amenorrhea), acne, hirsutism (dark hair on face, chin, or chest), weight gain, mood disturbances, acanthosis nigricans. | Rotterdam Criteria: Must meet 2 of 3—irregular cycles, hyperandrogenism, or polycystic ovaries on ultrasound. | Oral contraceptives (for cycle regulation), spironolactone (for hirsutism), metformin (for insulin resistance), weight loss. | Increased risk of diabetes, metabolic syndrome, endometrial hyperplasia, cardiovascular disease, and infertility. |
| Osteoporosis | Loss of bone density due to estrogen deficiency | Higher risk in postmenopausal women, especially those who are thin, Caucasian, or Asian, with lifestyle factors like smoking, excessive alcohol, low calcium/Vitamin D intake, and lack of weight-bearing exercise. | DXA scan: T-score < -2.5 (osteopenia: -1.0 to -2.4). Repeat every 1-2 years if on treatment, otherwise 2-5 years. | Bisphosphonates (e.g., alendronate, risedronate) to prevent bone resorption. Weight-bearing exercises, calcium + vitamin D supplementation. | Long-term bisphosphonate use linked to atypical fractures. Calcitonin has been associated with increased malignancy risk. |
| Condition | Cause | Signs & Symptoms | Diagnostics | Treatment | Concerns |
|---|---|---|---|---|---|
| Bacterial Vaginosis (BV) | Overgrowth of anaerobic bacteria in the vagina | Thin, homogeneous, white/gray discharge with a “fishy” odor, worsens after intercourse. No inflammation. Light gray discharge coating vaginal walls. | Wet mount: Clue cells, few WBCs. Whiff test (KOH) → fishy odor. Vaginal pH > 4.5. | Metronidazole (Flagyl) BID for 7 days or clindamycin cream. Not an STD—no partner treatment needed. Abstain from sex until treatment is completed. | Clue cells: Squamous epithelial cells with bacteria on borders. |
| Candida Vaginitis | Candida albicans yeast overgrowth | Thick, white, cottage cheese-like vaginal discharge with severe itching, redness, and swelling. | Wet mount: Pseudohyphae, budding yeast, large number of WBCs. | -azole antifungals: Fluconazole (Diflucan) oral, or topical options like miconazole (Monistat), clotrimazole, terconazole. Probiotics or yogurt may help. | Higher risk in diabetics, HIV patients, and those on antibiotics. |
| Atrophic Vaginitis | Estrogen deficiency | Vaginal dryness, irritation, itching, and pain during intercourse. Pale, thin vaginal tissue with reduced rugae, may bleed easily on exam. | Pap smear: Atrophic cellular changes. Elevated FSH/LH. Vaginal pH > 5.0. | Topical estrogen for symptoms or recurrent UTIs. Osphena (non-estrogen option). Oral estrogen alone is usually insufficient. | Common in postmenopausal women. |
| Dysmenorrhea | Excessive prostaglandin production | Primary: Pain begins with menstruation, improves over time and with NSAIDs. May have nausea, diarrhea, or back pain. Secondary: After age 35, worsens over time, abnormal bleeding, pain not midline (suggests endometriosis). | History and pelvic exam. Consider STI testing, check for fibroids or other pathology. | NSAIDs for pain relief. Exercise, heat therapy. Oral contraceptives may help. If secondary, treat the underlying cause. | Postmenopausal vaginal bleeding requires endometrial biopsy to rule out cancer. |
| Abnormal Uterine Bleeding (AUB) | Varies (PALM-COEIN classification) | Postmenopausal bleeding (>12 months since last period) → Requires OBGYN referral to rule out malignancy. | Evaluation depends on cause: History, imaging, labs. | Treatment depends on etiology: Hormonal therapy, surgical intervention, or addressing coagulation disorders as needed. | PALM-COEIN classification: Polyps, Adenomyosis, Leiomyoma, Malignancy, Coagulopathy, Ovulatory dysfunction, Endometrial disorder, etc. |
| Menopause | Natural cessation of menstrual cycles | No periods for 12 consecutive months. Symptoms include hot flashes, night sweats, and vaginal dryness. Often worsens before complete cessation. | Labs: ↑ FSH & LH, ↓ estradiol, testosterone, and progesterone. | Hormone therapy (low-dose estrogen/progestin) helps with symptoms but increases risk of breast cancer, endometrial hyperplasia, and CAD. Alternative treatments include SSRIs (venlafaxine, sertraline, paroxetine), gabapentin, phytoestrogens (soy, black cohosh, red clover), and high-dose vitamin E. | Perimenopause typically starts around ages 40-45. Hormone therapy should be used cautiously. |
Pregnancy
Pregnancy Milestones and Measurements
- Development Stages: Zygote → Blastocyst → Embryo → Fetus
- Calculating Due Date (Naegele’s Rule): Subtract three months from the first day of the last menstrual period (LMP), then add seven days (total pregnancy duration: 40 weeks or 280 days).
- Ultrasound Accuracy:
- First Trimester: Crown-rump length (margin of error: ±7 days)
- Second Trimester: Multiple fetal measurements (margin of error: ±10-14 days)
Uterine Growth & Landmarks
- Non-pregnant Uterus: Size of a lemon
- 8 Weeks: Comparable to an orange
- 10 Weeks: Size of a baseball, fetal heart tones (FHT) may be detected via Doppler
- 12 Weeks: Reaches just above symphysis pubis, about the size of a grapefruit (Doppler FHT detectable)
- 16 Weeks: Midway between symphysis pubis and umbilicus
- 16-18 Weeks: Quickening (first fetal movements felt)
- 20 Weeks: Fundus at umbilicus (FHT detectable via stethoscope)
- 20-36 Weeks: Fundal height typically matches gestational weeks in centimeters (±1 cm)
- At Term: Fundal height drops as the baby engages in the pelvis
Concern: If the uterus measures smaller than expected, consider intrauterine growth restriction (IUGR).
Risk Factors for Ectopic Pregnancy
- History of:
- Salpingitis (inflammation of the fallopian tubes)
- Previous ectopic pregnancy
- Tubal surgery or damage
- Pelvic inflammatory disease (PID) or prior cervicitis
- Infertility or assisted reproductive techniques (e.g., IVF)
- Other contributing factors:
- Cigarette smoking
- Progestin-only contraception
- Current intrauterine device (IUD) use
- Tubal ligation failure
Diagnosis Considerations:
- If hCG > 1500 but ultrasound does not confirm an intrauterine pregnancy, suspect ectopic.
- Treatment options: Methotrexate (medical management) or surgical intervention if necessary.
Dietary Requirements
- Pregnancy: Increase intake by 300 kcal/day
- Breastfeeding: Requires an additional 500 kcal/day
- Calcium: 1000-1500 mg/day to support bone health
- Folic Acid: 0.4-1 mg/day (found in leafy greens and fortified cereals) to aid in fetal development
Healthy Weight Gain During Pregnancy
| BMI Category | BMI Range | Recommended Weight Gain (lbs) |
|---|---|---|
| Underweight | Less than 18.5 | 28 – 40 |
| Normal Weight | 18.5 – 24.9 | 25 – 35 |
| Overweight | 25.0 – 29.9 | 15 – 25 |
| Obese | 30 or higher | 11 – 20 |
Twin pregnancy: Higher recommended weight gain (37–54 lbs).Postpartum weight loss: Expect to shed 20–30 lbs within the first few weeks.Food precautions: Avoid soft cheeses, raw or undercooked meats, and unpasteurized milk.Seafood caution: Refrain from consuming raw shellfish or oysters due to the risk of Vibrio vulnificus infection.Deli meats warning: Cold cuts, uncooked hot dogs, and deli meats pose a risk of Listeria monocytogenes contamination.Caffeine intake: Limit to an 8 oz cup of regular coffee.Weight gain pattern: The majority of weight is gained in the third trimester, averaging 1–2 lbs per week.
Asymptomatic bacteriuria
Always requires treatment (3 days if asymptomatic, 7 days if symptomatic).First-line antibiotics:
- Nitrofurantoin (Macrobid) – BID for 5–7 days
- Amoxicillin/Clavulanate (Augmentin) – BID for 3–7 days
- Amoxicillin – BID for 3–7 days
- Cephalexin – BID for 3–7 days
Medication precautions: Avoid nitrofurantoin and sulfa-based drugs near term, during labor, and postpartum.Neonatal risk: Increased hyperbilirubinemia, leading to kernicterus.Pregnancy consideration: A urinary tract infection (UTI) during pregnancy is classified as a complicated UTI.
Indicators of Pregnancy
Definitive (Positive) Signs
- Fetal palpation by a healthcare professional
- Ultrasound confirmation of fetal presence
- Detection of fetal heart tones:
- Doppler: 10–12 weeks
- Fetoscope/Stethoscope: 20+ weeks
Likely (Probable) Signs
- Goodell’s Sign (4 weeks): Cervical softening
- Chadwick’s Sign (6–8 weeks): Bluish discoloration of the cervix and vagina
- Hegar’s Sign (6–8 weeks): Softening of the uterine isthmus
- Uterine enlargement
- Ballottement: A bouncing sensation of the fetus when pushed, felt through vaginal examination
- Positive urine hCG (may also indicate molar pregnancy or ovarian cancer)
Possible (Presumptive) Signs
- Missed periods (amenorrhea)
- Nausea and vomiting
- Breast tenderness and changes
- Fatigue
- Frequent urination
- Slightly elevated basal body temperature
- Quickening (16 weeks): First sensation of fetal movement by the mother
Miscellaneous Insights
- Zika Virus: Associated with cleft palate; highest risk occurs during the first trimester.
- Prenatal Visit Schedule:
- Every 4 weeks up to 28 weeks
- Every 2 weeks from 28 to 36 weeks
- Weekly visits from 36 weeks until delivery
- Placental Drug Transfer:
- Substances <500 daltons can cross the placenta
- Molecules >1000 daltons typically cannot pass
- Asthma in Pregnancy:
- Increased risk of bronchospasms between 36 and 40 weeks
Laboratory Tests During Pregnancy
- Urinalysis: Performed at every prenatal visit
- Alkaline Phosphatase: Always elevated due to fetal bone development
- Leukocytosis with Neutrophilia: A normal physiological response
- Alpha-Fetoprotein (AFP) Screening (16-20 weeks):
- Low AFP: Further evaluation with a triple screen to assess for Down syndrome
- High AFP: Rule out neural tube defects or multiple gestation with an ultrasound
- Triple Screen Test: Measures AFP, beta hCG, and estriol
- Quad Screen Test: Adds inhibin A to the triple screen, improving detection of Down syndrome
- Amniocentesis: Gold standard for diagnosing genetic disorders via fetal chromosome/DNA analysis (1 in 400 risk of fetal loss)
- Genetic Carrier Screening:
- Tay-Sachs Disease: Common in Ashkenazi Jewish populations
- Cystic Fibrosis: More prevalent among Caucasians
- Sickle Cell Trait: Primarily affects individuals of African descent
Prenatal Lab Schedule
- First Prenatal Visit:
- Confirm pregnancy with hCG
- Screen for Pap smear, gonorrhea/chlamydia
- Check rubella, varicella, rubeola immunity
- Test for syphilis, HIV, HBsAg (consider HCV screening)
- CBC, blood type, antibody screen
- TSH if thyroid disease is being treated
- 16-20 Weeks:
- Quad Marker/Screen for chromosomal and neural tube abnormalities
- 24-28 Weeks:
- Gestational diabetes screening
- 28-32 Weeks:
- Repeat STI screening
- Administer RhoGAM if the mother is Rh-negative
- 32-36 Weeks:
- Assess fetal position
- Monitor fetal well-being with kick counts
- 35-37 Weeks:
- Group B Streptococcus (GBS) culture
- If positive: Administer Penicillin G (5 million units IV, then 2.5-3 million units every 4 hours until delivery)
- 40-42 Weeks:
- Vaginal examination to evaluate cervical ripeness before labor induction if necessary
Physiological Adaptations in Pregnancy
- Cardiovascular Changes:
- Heart shifts forward and to the left
- Heart rate increases by 15-20 BPM
- Heart sounds become more pronounced; S3 is common, and S2 splitting may be noticeable
- Systolic ejection murmur (Grade II/IV) over pulmonary and tricuspid areas
- Cardiac output rises by 30-50% (↑ preload), while systemic vascular resistance and blood pressure decrease (↓ afterload)
- Plasma volume expands by 50%, leading to physiological anemia
- Uterine compression of the inferior vena cava can cause orthostatic hypotension
- Hypercoagulable state, increasing the risk of clot formation
- Respiratory System:
- Basal rales present but clear with coughing
- FEV1 remains unchanged, but total lung capacity decreases
- Gastrointestinal Changes:
- Constipation and heartburn due to hormonal effects and pressure on the digestive tract
- Skin and Pigmentation:
- Increased melanocyte-stimulating hormone causes:
- Linea nigra – dark line extending down the abdomen
- Darkening of the nipples and areolas
- Chloasma (melasma): Blotchy hyperpigmentation on forehead, cheeks, nose, and upper lip
- More common in individuals with darker skin
- Linked to elevated estrogen levels
- Striae gravidarum (stretch marks)
- Increased melanocyte-stimulating hormone causes:
- Hair and Nails:
- Telogen effluvium (postpartum hair loss) due to hormonal fluctuations
- Renal System:
- Kidney size increases
- GFR rises due to increased cardiac output and renal perfusion
- Vascular and Circulatory Effects:
- Nasal congestion and nosebleeds (epistaxis) from increased blood flow
- Varicose veins due to vascular relaxation and increased venous pressure
- Peripheral edema from fluid retention and circulatory changes
Pregnancy History Overview
- Total Pregnancies (Gravida)
- Full-Term Births
- Preterm Deliveries
- Pregnancy Losses (Miscarriages/Abortions)
- Living Children
Medication Safety in Pregnancy
- Category A – Proven Safe
- Vitamin A, Levothyroxine
- Category B – Generally Safe
- Penicillins, Cephalosporins, Macrolides, Acetaminophen, Pulmicort, Maalox, Colace
- Methyldopa (Monitor LFTs—discontinue if jaundice, abnormal LFTs, or unexplained fever)
- Calcium Channel Blockers (Procardia), Beta-Blockers (Labetalol), Insulin
- Category C – Likely Safe
- Sulfonamides (avoid in the third trimester), Clarithromycin
- NSAIDs (risk of premature ductus arteriosus closure)
- Category D – Potential Risk
- ACE Inhibitors, ARBs, Quinolones, Tetracyclines, Tegretol, Depakote
- Fluoxetine, Paroxetine
- Category X – Unsafe
- Accutane, Thalidomide, Statins, Proscar, Misoprostol, Evista
- Teratogenic Risks
- Alcohol – Fetal Alcohol Syndrome (FAS)
- Aminoglycosides – Hearing loss
- Smoking – Intrauterine Growth Restriction (IUGR)
- Cocaine – Increased risk of stroke (CVA)
- Isotretinoin (Accutane) – Severe birth defects
- Lithium – Congenital heart defects
- Gestational Diabetes – Large for Gestational Age (LGA), neural tube defects
Miscellaneous Pregnancy Insights
- Toxoplasmosis Risk – Avoid cat litter and raw or undercooked meat.
- Harmful Substances – Smoking (linked to intrauterine growth restriction) and alcohol should be avoided.
- Heat Exposure – Refrain from using hot tubs, saunas, or prolonged exposure to high temperatures.
- Heartburn Causes – Progesterone and calcium channel blockers (CCBs) relax the esophageal sphincter, contributing to acid reflux.
- Uterine Involution – Postpartum contractions last 2-3 days. A soft, boggy uterus with excessive bleeding indicates uterine atony (poor contraction). Full involution takes about six weeks, with breastfeeding accelerating the process.
- Edwards Syndrome (Trisomy 18) – A genetic condition associated with severe developmental abnormalities.
| Condition | Cause | Signs & Symptoms | Diagnostics | Treatment | Concerns |
|---|---|---|---|---|---|
| Placental Abruption (Abruptio Placentae) | Late third-trimester pregnancy with sudden-onset vaginal bleeding, painful contractions, and a firm, rigid uterus. Up to 20% may not have visible bleeding. | CBC, PT/PTT, blood typing & crossmatching, Rh testing, ultrasound | Immediate delivery of the fetus; severe cases can lead to maternal hemorrhage. | Increased risk with hypertension, preeclampsia, cocaine use, or prior history of placental abruption. | |
| Placenta Previa | Painless vaginal bleeding in the late second or third trimester, often worsened by intercourse. Soft, non-tender uterus. | Bed rest, magnesium sulfate for cramping. Mild cases may resolve with reimplantation. No vaginal or rectal exams. If cervical dilation or hemorrhage occurs, delivery via C-section. | Higher risk in those with a history of C-sections, multiple pregnancies, older age, smoking, fibroids, or cocaine use. | ||
| Preeclampsia | Unknown; risk factors include first pregnancy, multiple pregnancies, age >35, obesity, prior history, hypertension, or kidney disease. | Sudden-onset recurrent headaches, blurred vision, scotomas, facial/hand edema, and rapid weight gain in late third trimester (>34 weeks). New-onset right upper quadrant pain, nausea, vomiting. Blood pressure >140/90 with proteinuria (1+ on dipstick), oliguria. If seizures occur, it progresses to Eclampsia. | Diagnostic criteria: Triad of hypertension, proteinuria, and edema. BP >140/90 after 20 weeks. Proteinuria >0.3g/24hr. Facial/hand swelling. | Delivery (can occur up to four weeks postpartum). | Hypertension before 20 weeks is considered chronic hypertension, not preeclampsia. |
| HELLP Syndrome (Hemolysis, Elevated Liver Enzymes, Low Platelets) | Rare but severe complication of preeclampsia/eclampsia. | Sudden onset of preeclampsia symptoms with severe worsening. | Elevated AST, ALT, LDH, total bilirubin >1.2, platelets <100,000, decreased hemoglobin/hematocrit. | More common in multiparous women over 25. | |
| Rh Incompatibility | Rh-negative mother carrying an Rh-positive fetus. | If untreated, the maternal immune system develops antibodies against Rh-positive blood, leading to fetal hemolysis in subsequent pregnancies. | Coombs test: Indirect detects maternal Rh antibodies; direct detects antibodies in the infant. | RhoGAM (anti-D immune globulin) prevents maternal sensitization. Given at 28 weeks and within 72 hours postpartum. | Failure to administer RhoGAM can lead to hemolytic disease in future pregnancies. |
| Gestational Diabetes | Increased risk of neural tube defects, congenital heart disease, macrosomia (large baby), birth trauma (shoulder dystocia), preeclampsia, polyhydramnios, and neonatal hypoglycemia. Risk factors include obesity, family history, ethnicity (Asian, Native American, Black, Hispanic, Pacific Islander), previous large infant (>9 lbs.), and maternal age >35. | Screening: Early screening for high-risk individuals; routine screening at 24-28 weeks. If diabetes is diagnosed in the first trimester, it is classified as Type 2 Diabetes. Postpartum testing at 6-12 weeks and every 3 years. Diagnostic criteria: One-step method: 75g OGTT – fasting >92, 1-hour >180, 2-hour >153. Two-step method: 50g OGTT (non-fasting), if 1-hour >140, proceed to 100g OGTT. Fasting >95, 1-hour >180, 2-hour >155, 3-hour >140. Target glucose: Preprandial ≤95, 1-hour <140, 2-hour <120. A1C goal: 6.0-6.5%. | Lifestyle modifications, insulin, glyburide, or metformin if needed. | Increased risk of Type 2 Diabetes later in life. |